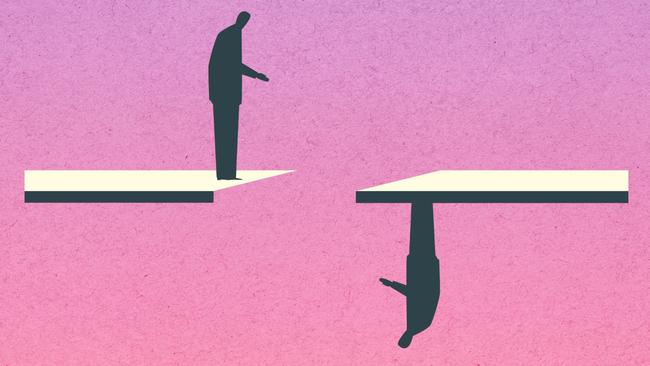
The mentally ill were once housed in asylums, now they’re on the streets
Since the closure of mental asylums, the ranks of prisoners and the homeless have swelled with the severely mentally ill.

The tranquil gardens of Rozelle Hospital, Sydney’s main asylum for the severely mentally ill until it closed in 2008, are what 70-year-old Craig remembers most about that bygone era of institutionalisation.
Undeniably, there were horrors within the hospital’s walls in a model of care that stripped patients of autonomy and subjected them routinely to restraint and seclusion that was hardly therapeutic and often cruel.
But for many of those cast adrift as the long-term mental hospitals shut down, life outside of the institutions’ walls has offered little comfort either.
“No one gives a f..k about me to be honest,” says Craig.
“I haven’t had any help from anyone. No one has assisted me at all. It’s hard to trust anyone.”
Craig was a frequent inpatient at Rozelle. Since the asylums were cleared out, he’s spent most of the past 30 years homeless, apart from years spent in jail. It’s a not infrequent trajectory for those who were promised community supports would replace institutional care – something that never happened at scale in the beginning, and the little support there was initially eroding severely over time.
We find Craig at Town Hall in the heart of Sydney’s CBD, where he spends much of his week idling outside of the city’s Woolworths store. On this city block of skyscrapers and high-end retail shops, Craig is one of the perkier street dwellers. Most are asleep beneath blankets on this glaringly bright spring day, ignored by the office workers who bustle by.
Many people living on the streets have complex mental health conditions, but are rarely reached by mainstream healthcare services let alone housing support.
The homeless are visible on the streets of every city in the nationney . Those in prison, however, are hidden away, as are those that society has no place for other than involuntary mental health inpatient wards. Psychiatrists at public hospitals in Sydney and Melbourne told The Australian they have patients who have been on their wards for more than 700 days.
It’s often forgotten that the landmark 1993 report by the nation’s first human rights commissioner, Brian Burdekin, who documented human rights transgressions in institutional care, recommended long-term care be available for the most vulnerable of the severely mentally ill who could not be cared for in the community. As did the NSW Richmond report a decade earlier.
Those recommendations were ignored, money never followed patients, and corresponding to the closure of mental institutions, the ranks of prisoners and the homeless swelled with the severely mentally ill.
The proportion of prisoners with schizophrenia alone is at historic highs: in NSW it’s about 8 per cent of inmates. That compares with a rate of 1 per cent across the wider community.
“I think our use of prisons are as kind of asylums,” says Sydney psychiatrist Olav Nielssen, who has just opened a supported accomodation facility in Sydney’s inner west called Habilis. “Jails are currently the biggest mental health service in the state of NSW for psychotic illnesses.”
Despite that, mental healthcare in prisons nationwide is threadbare.
The ratio of mental health worker positions in jails is critically low in comparison to need.
The majority of those with mental illness are incarcerated on remand or short sentences for petty crimes. They are released to homelessness, then frequently end up back in prison.
“The release of people from prison is probably one of the worst-managed services I’ve ever come across,” says Yvonne Bonomo, director of addiction medicine at St Vincent’s Hospital in Melbourne. “People maybe get two nights in a hotel to then follow up with a GP, and it all falls apart relatively quickly. Their mental health deteriorates, their substance use escalates, and they often just end up right back in prison.

“And if people complete their whole sentence, they don’t get any support at all upon discharge. It’s only if they’re on parole, they’re given support in the community.”
Federal health minister Mark Butler issued thanks to the writer at The Australian publishing a major mental health series this week on the neglect of those with severe needs, saying this cohort were “getting a really raw deal in our community” and had been in the 30 years since deinstitutionalisation of long-term asylums.
“The sorry fact is that deinstitutionalisation wasn’t followed up with the sorts of community-based investments that were needed to give proper support to those people,” Mr Butler said. He said about 230,000 people were getting zero psychosocial supports. Health ministers will address that issue next in February next year. “This is a cohort that is largely outside the NDIS. I think the attention that The Australian series is drawing to that cohort is welcome, because this has been kept in the shadows for far too long.”
In NSW, an estimated 63 per cent of the prison population has a mental health diagnosis; countless more are undiagnosed. Among juveniles the figure is as high as 83 per cent.
Nationally those with mental illness make up at least 40 per cent of the jail population.
Mental health: Cast Adrift

Home truths: jails overflow as mentally ill live on the streets
Since the closure of mental asylums, the ranks of prisoners and the homeless have swelled with the severely mentally ill.

‘Nowhere to go’: supported housing could ease the burden of mental illness
Investments in housing for those with severe mental illness would reap enormous gains and savings for the nation.

Shocking plight of mentally ill ‘a stain on nation’
Health Minister Mark Butler describes the atrocious health outcomes, social exclusion and widespread homelessness as ‘a shocking reflection on our community’. The situation is revealed in a report by The Australian and Australian National University.

The clearing out of asylums was meant to provide hope. Instead it spawned an underclass
The severely mentally ill were promised a better future after asylums were mothballed. The promises were hollow.

‘My nightmare of trauma and terror’
I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system. This is my story.
Shocking life expectancy gap has not shifted in a century
The huge gap in life expectancy between those with severe mental illness and the rest of the population is growing in Australia, with no improvement in sight.

‘As a father I’m heartbroken, as a taxpayer I’m appalled’
Patrick Leunig went to a top private school and was set to study law. Then his life spiralled downwards. His grief-stricken father tells of how our system failed his son.

Freedom fight: Locked up and invisible in the heart of Australia
A young Aboriginal man’s escape from hell charts a community win for one of the many cognitively impaired and mentally troubled First Nations offenders who languish in our prison system.

Australia has a chance to fix its mental health system. Will we take it?
Australia’s broken mental health system has failed hundreds of thousands of people with severe illness with ineffective care – and that’s if they can access any at all. But one initiative may shift the dial.

‘The mental health ward became my prison cell’: a patient’s plea for change
Billie spent more than 1000 days in hospital before she turned 18. Damaged but determined, she is now speaking out for mental health reform.
Forensic mental health units nationwide are heaving. In NSW patients sometimes spend as long as four years in prison awaiting a bed in a forensic health facility – much longer, in many cases, than they would have been incarcerated had they been convicted of a crime.
In the Northern Territory, there are barely any forensic healthcare beds and many of those found unfit to plead on the basis of mental illness are held in maximum security prisons.
People with a mental health condition are also one of the fastest-growing groups of clients accessing specialist homelessness services. In 2020-21 in NSW, a third of people who sought such support had a current mental health condition, up from 19 per cent a decade ago.
According to the Productivity Commission, when substance-use disorders are excluded, about a third of the homeless population has mental illness. For those at the severe end of the spectrum, the percentage is much higher.
It all comes at vast cost to taxpayers. The cost can range from $1m for young people over the course of their adolescence to as high as $5.5m when police, juvenile justice, welfare, housing, health and legal aid services are taken into account, according to a University of NSW analysis.
Australia spends about $4.9bn a year to house people in prisons. As much as $1.1bn of that expenditure by the criminal justice system can be attributed to mental illness.
The cost of providing community support and healthcare to the mentally ill to break the cycle of homelessness and imprisonment would be orders of magnitude less, says Dr Nielssen.
“It’s not costly at all, that’s the absurdity of it,” he says. “And despite literally hundreds of millions of dollars in hospital care alone, the health outcomes for people with severe mental illness are terrible, they’re very poorly treated. There’s no continuity of care. There’s premature mortality. It’s just an absurd waste of resources.
“You could fully house people for a fraction of the cost, and they’d be very much better off health wise.
“From an economic point of view, it’s so costly and wasteful to not look after people a little better.
“That’s just the economic argument.
“The moral argument ... is that for one of the richest societies in history, the river of money that’s flowed through Australia hasn’t flowed to just a little bit of care for the most disadvantaged.”


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout