‘As a father I’m heartbroken, as a taxpayer I’m appalled’: a family’s mental health ordeal laid bare
Patrick Leunig went to a top private school and was set to study law. Then his life spiralled downwards. His grief-stricken father tells of how our system failed his son.

In the maternity ward of the Ashford Hospital in Adelaide, Patrick Leunig arrived with a roar. Father Andrew stood in scrubs as time slowed down and his first child was lifted out of the womb.
“There was what seemed like an eternal silence,” Mr Leunig recalls.
“Then Patrick let out what I could only describe as a roar, like a tiger cub. I fumbled my way through the first weeks of fatherhood with obvious pride, care and affection but, oh boy, the first time that kid smiled at me, I felt a greater love than I’d ever felt before.”
Sometimes, love is not enough.
A happy childhood, a flourishing teenage academic life in one of Adelaide’s top private schools, and a coveted place in a law and economics degree were all laid to waste in eight years as Patrick Leunig transitioned to adulthood.
“We all thought that he was a magnificent rocket just resting on the launch pad, ready for launch,” his father says.

But mental illness does not discriminate, neither by intelligence, nor wealth. Nationally, it accounts for the second-biggest burden of disease, and as a major reporting series by The Australian in conjunction with the Australian National University has shown, there is vast, unmet need in the provision of healthcare, housing and social supports for those severely affected.
For many, it’s not just a matter of not getting healthcare and supportive social services. It’s a matter of not living past the age of 65. Or barely living at all.
The life expectancy gap between those with severe mental illness stands at 17 years and has not narrowed in a century – in fact it’s widened.
“This wealthy, sophisticated country needs to do a lot better,” says Mr Leunig.
“I have skills, money and connections – and trying to navigate Australia’s mental health system still managed to defeat me.”
The first inkling that something was not right came in Patrick’s first few months at university. While his peers languished in the sun on lecture breaks on green university lawns, the teenager holed up in his bedroom at home with the curtains drawn. Within four months, he had dropped out of uni. A couple of years of “drifting” between casual jobs amid increasingly poor mental health combined with cannabis use culminated in crisis in 2019, when Patrick’s beautiful mind descended into psychosis. His father called the community mental health team, and in August 2019, a psychiatrist attended Patrick’s home with three police officers and a trio of nurses in tow. Patrick was unwilling to engage, and an order for involuntary treatment at a mental health facility was issued. He was handcuffed and forcibly injected.
“I don’t suppose that any parent is ever happy to see their child in handcuffs, but I was relieved,” Mr Leunig says.
“He was safe and we were at the beginning of whatever was to come next.”

Sadly, what came next was nothing short of “rolling chaos”. Five hospitalisations totalling 199 days and an eventual diagnosis of schizoaffective disorder. Five years of insecure housing and homelessness – Patrick’s behaviour made living with his family impossible. The hospital system was a “revolving door”. Patrick would sometimes spend as long as 72 hours in the emergency department, an environment of “utter chaos”. He was repeatedly discharged from inpatient wards, often after only a day or two, when still clearly unwell, he’d walkout of the ward in a manic state with only a garbage bag containing his few clothes, and nowhere to go.
Once, defeated staff told Mr Leunig his son had been hurriedly discharged on the order of “some executive” to “find some beds”.
There was no pathway whatsoever in the health system to address his substance abuse – a common story for those with comorbid addiction and mental health disorders.
“The obvious reality is that Patrick was neither ‘well’ nor ‘calm’ at any time when he was discharged from hospital,” says his father.
“We tried to help him. And with the benefit of hindsight, I would have done some things differently. But, Jesus, what do you do?”
Patrick’s young adult life was a vivid illustration of the ineffective nature of Australia’s mental health system and its failure to co-ordinate with either substance-abuse services or vital housing services. Such assistance is almost non-existent, especially since the advent of the NDIS, which left many severely mentally ill people out in the cold as existing services were wrapped into the scheme and state governments stepped back.
The terrible tragedy is that his parents could see what was coming as they desperately tried to get help for their son.
“His mother was the first one to say it out loud,” Mr Leunig says.
“She said to me at one point: ‘you know, we’re going to lose him’.”
Mr Leunig’s emails over the course of 20 months to South Australia’s guardianship authority, which failed to lodge an NDIS application for him despite many entreaties, now read as achingly prophetic.
“What is the next step?” Mr Leunig asked staff in February 2023. “Prison? Or worse?”
Then in March, as Patrick was yet again discharged from hospital to nowhere: “If we cannot solve the housing problem he will be dead or in prison. I can’t see any other likely outcomes. “Are there any managed facilities below prison that might work?”
“I am despairing that this downwards spiral continues,” he wrote.
Again, later that month, Mr Leunig observed: “Under the current scenario there is no prospect of proper recovery and a real prospect of a tragic but preventable end”.
For patients like Patrick, acute inpatient treatment is nothing but a temporary bandaid. When ejected onto the streets, there is nothing except enforcement of crude orders. The work of community teams – which were supposed to provide support when Australia’s state-based asylums for those with severe mental illness were progressively shut over the last decades of the last century – now consists largely of enforcing compulsory medication regimes for those on community treatment orders. Therapy in the private sector is far too expensive and inaccessible for many of the severely mentally ill, even if they are willing patients.
Mr Leunig’s despair at his son’s plight was acute, but the business consultant also became increasingly aware over time of the sheer fiscal waste in the microcosm in his son’s case.
“I calculate that the total cost of supporting Patrick from August 2019 to March 2024, including police, ambulances, hospitals, community health care and guardianship exceeded $750,000,” Mr Leunig tells The Australian.
“This is serious money but it was mainly spent in a reactive fashion, akin to the ambulances parked at the bottom of the cliff.
“The very idea of throwing someone who is still suffering a degree of mental distress into a taxi with two nights in a motel is disgraceful.
“We don’t blame the system for Patrick’s death. But we felt that failings in the system increased and prolonged his trauma and that ultimately made his life, and ours, much more difficult than it needed to be and the path to wellness and living his best life that much harder” - Andrew Leunig
“It seems to me that even acute treatment in mental health hospitals is the administration of medication (a few minutes a day) and then a lot of waiting and observation. Continue the medication or tweak it. Rinse and repeat. The inpatients have little if anything to do.
“The hospital has merely passed the parcel. It then creates a crisis for the people charged with finding accommodation for that person.
“There is also bed blockage arising from older citizens waiting for aged care beds to become available – are they being shunted into taxis too? I don’t think so. The harsh reality is that there is not enough accommodation available.”
Mental health: Cast Adrift

Home truths: jails overflow as mentally ill live on the streets
Since the closure of mental asylums, the ranks of prisoners and the homeless have swelled with the severely mentally ill.

‘Nowhere to go’: supported housing could ease the burden of mental illness
Investments in housing for those with severe mental illness would reap enormous gains and savings for the nation.

Shocking plight of mentally ill ‘a stain on nation’
Health Minister Mark Butler describes the atrocious health outcomes, social exclusion and widespread homelessness as ‘a shocking reflection on our community’. The situation is revealed in a report by The Australian and Australian National University.

The clearing out of asylums was meant to provide hope. Instead it spawned an underclass
The severely mentally ill were promised a better future after asylums were mothballed. The promises were hollow.

‘My nightmare of trauma and terror’
I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system. This is my story.
Shocking life expectancy gap has not shifted in a century
The huge gap in life expectancy between those with severe mental illness and the rest of the population is growing in Australia, with no improvement in sight.

‘As a father I’m heartbroken, as a taxpayer I’m appalled’
Patrick Leunig went to a top private school and was set to study law. Then his life spiralled downwards. His grief-stricken father tells of how our system failed his son.

Freedom fight: Locked up and invisible in the heart of Australia
A young Aboriginal man’s escape from hell charts a community win for one of the many cognitively impaired and mentally troubled First Nations offenders who languish in our prison system.

Australia has a chance to fix its mental health system. Will we take it?
Australia’s broken mental health system has failed hundreds of thousands of people with severe illness with ineffective care – and that’s if they can access any at all. But one initiative may shift the dial.

‘The mental health ward became my prison cell’: a patient’s plea for change
Billie spent more than 1000 days in hospital before she turned 18. Damaged but determined, she is now speaking out for mental health reform.
By late last year, Patrick had finally gained a place in a rare supported accommodation facility, at Common Ground in Adelaide. Deep connections with peers had helped dissolve his denial and accept his chronic illness. His mates looked out for him. He was the happiest he had been for years.
But for the vulnerable, demons lurk, and strike at unexpected moments. So it was on the eve of the this year’s Easter long weekend.
As Mr Leunig prepared to leave Adelaide for a beachside break, he dropped in to Common Ground and delivered a small gift and card to his son ahead of Patrick’s 26th birthday. On the day, he sent a text: “Happy birthday son. Hope that you have a great day. Love Dad”.
On Easter Monday at 9.30am, Mr Leunig received a call from the Port Adelaide police. “A horrible feeling washed through me,” he says. “This was a call that I’d been fearing but hoping that wouldn’t ever come.”
Patrick was dead. Just when he had finally gained some stability, he had overdosed on methamphetamine in his room. By his father’s best guess, it was accidental. The facts of Patrick’s case are before the South Australian coroner.
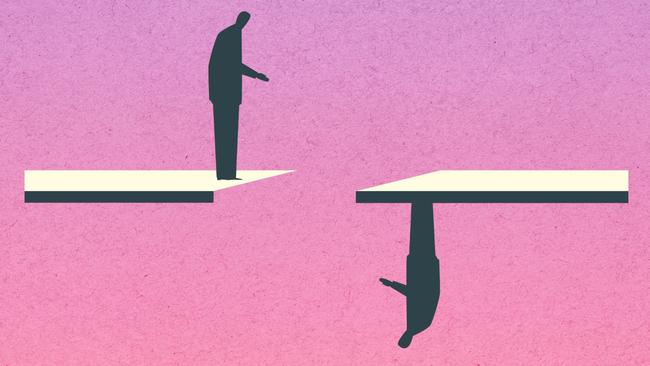
“Patrick had been running along a tightrope for years,” Mr Leunig says. “And now he’d fallen just when I felt like there were some green shoots.
“But I think that we’d all had a feeling that this day may come. He’d largely been lost to us for a number of years. We all held out hope that he’d receive care and that we could repair and re-engage. Where there’s life, there’s hope, but now there was no life and no hope.
“As a father – I’m heartbroken. As a citizen and a taxpayer, I’m appalled.
“We don’t blame the system for Patrick’s death. But we felt that failings in the system increased and prolonged his trauma and that ultimately made his life, and ours, much more difficult than it needed to be and the path to wellness and living his best life that much harder.”

A memorial service attended by 170 people on April 12 gave Patrick Leunig a standing ovation. The odds stacked against him, he did the best he could.
“A number of people have thanked me for being brave in openly sharing details about Patrick’s illness and substance abuse disorder,” Mr Leunig says. “If anyone was brave it was Patrick.”
When the grieving father made the sad trek to Patrick’s place of death a few days after Easter, the young man’s meagre possessions were returned. They largely consisted of a cherished small electric piano, and a lounge that had taken pride of place in his room – the only piece of furniture he owned.
Also among the possessions was Patrick’s unopened birthday card from his father.
“Patrick had never received it,” Mr Leunig says. “The card read: ‘I love you. Always have, always will’.”
FOR SUPPORT PLEASE CALL
Lifeline: 13 11 14, lifeline.org.au
SANE Support line and Forums: 1800 187 263, saneforums.org
Headspace: 1800 650 890, headspace.org.au
Beyond Blue: 1300 224 636, beyondblue.org.au


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout