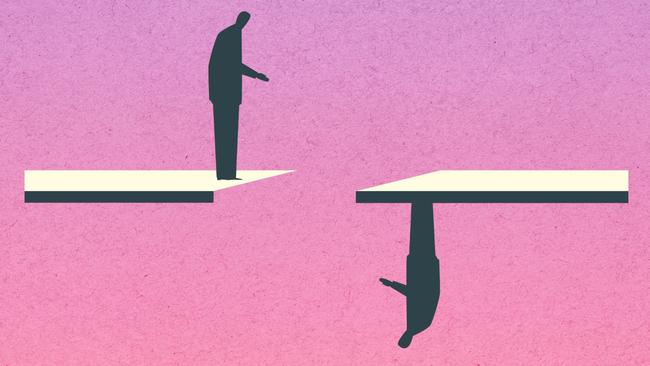
Seclusion, degradation and trauma: living with schizophrenia in a broken mental health system
I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system. This is my story.

I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system.
When I was 15, I was first sectioned following a suicide attempt. The psychiatrist who made this decision physically restrained me and painfully kept my hands behind my back because I called him a “bitch”. I realise now that this is inappropriate language; however, his reaction was far more inappropriate. I was in seclusion for two hours and this was the time that I began to realise that even though I was in hospital, I may not be safe.
This was the beginning of many years of different psychiatrists, treatments, diagnoses, wards, hospitals and medications. When an individual is sectioned, they are stripped of their basic rights and treated unfairly. In my experience, people are forced to suffer through the following:
• Not able to use bathroom freely, instead using a silver bowl, similar to a prison cell.
• Male staff or security pulling down your pants for IM (intra-muscular needle into buttock). It is difficult to put this experience into words but as a woman it made me feel unsafe, unprotected and disrespected. I was not given any choice regarding the gender of the staff member in this situation.
• Seclusion is a very traumatising experience which still impacts me to this day, more than 10 years later. It is a situation in which I am forced to stay inside my head as I have no stimulation and would sometimes need to punch a wall to force myself outside of my head. In my opinion, once sedative medication has taken effect, an individual does not need to remain in seclusion as the reason for their behaviour has been counteracted.
• Seclusion should be utilised as a tool for medication to take effect in safety rather than as a form of treatment or punishment. There should be policies against keeping people in seclusion for long periods.

My experience of the public mental health system has been varied. While there have been times that I have had the opportunity to meet very nice and experienced nurses and doctors, it is the many negative experiences that continue to impact me after all this time.
I recently experienced a mental health crisis and went to St Vincent’s Hospital in Sydney. I was in hospital in the SAS (Safe Assessment Space) unit for five days and four nights while waiting for a bed. The entire unit was at capacity and there were another nine patients waiting to be admitted. This is an example of the poor doctor-to-patient ratio across emergency departments and demonstrates the pressure that staff are under to move people along, which means that they are unable to give the proper care that each patient needs and deserves.
In my experience, patients who have been given a “difficult” diagnosis, such as borderline personality disorder (BPD), receive very different treatment to those with a diagnosis such as depression. It was almost like a hierarchy of difficulty that would determine how nice or caring staff would behave towards you.

It should also be noted that so many of these diagnoses are later revised and found to be incorrect, such as what happened to me because doctors were not able to take time to get to know me or my situation well enough. I have been given diagnoses of depression, anxiety, OCD, bipolar, schizoaffective disorder and BPD at one point before being diagnosed with schizophrenia. I was treated so differently at each stage with each different diagnosis.
In an adolescent ward I have spent time in, each patient is considered on a different “level” of behaviour that will determine which privileges they can or cannot have access to. For example, after an incident of self-harm, staff will slowly take away personal items (more items each time the behaviour occurs), even those that could not be used to self-harm. They would even go so far as to take away personal clothing, leaving patients in only a heavy gown (seclusion gown made of heavy anti-ligature material with thick stitching). These items would be removed for 24 hours, or until the staff decide that you have started to “behave”.
There was once an incident where a room search was being conducted, and staff found and read through my personal diary. This made me feel angry and disrespected.
Also, during my stay at this hospital I was forced to stay in the adult ward even though I was only 16, because staff wanted to “show me a lesson” to demonstrate what would happen if my “behaviour” continued. I still remember how I was taken there; the staff were very aggressive, and my experience was horrific.
Mental health: Cast Adrift

Home truths: jails overflow as mentally ill live on the streets

‘Nowhere to go’: supported housing could ease the burden of mental illness

Shocking plight of mentally ill ‘a stain on nation’

The clearing out of asylums was meant to provide hope. Instead it spawned an underclass

‘My nightmare of trauma and terror’
Shocking life expectancy gap has not shifted in a century

‘As a father I’m heartbroken, as a taxpayer I’m appalled’

Freedom fight: Locked up and invisible in the heart of Australia

Australia has a chance to fix its mental health system. Will we take it?

‘The mental health ward became my prison cell’: a patient’s plea for change
In 2020, when I was in hospital, I wrote a letter about my experiences and did my best to pass it on to the right people. However, they never replied to my letter and so I assume did not take me seriously or feel that I should be acknowledged. (I have included the letter herein.)
There were many times during my numerous hospitalisations that I felt I was not being taken seriously and even being ignored. For example, the diagnosis of severe dystonia that I got in my neck was treated as though I was “faking it”. This also happened when I began hallucinating from medication and when I would faint due to low blood pressure. I remember a specific incident when I fainted in front of a group of hospital staff and they did not come to my aid. This type of attitude towards me happened in most wards; however, in adolescent wards I was accused of “attention seeking”, being “naughty”, having a “tantrum”, and “trying to be the most unwell on the ward” as though my suffering was not genuine.
My experiences, and the experiences of the people around me, should be enough to show that there is a desperate need for change in the public mental health system.
If the necessary changes were to happen, then someone like me would experience respect, fairness and the correct treatment.
*Billie is a pseudonym used to protect her privacy.
