Mark Butler: Shocking plight of the mentally ill ‘a stain on our nation’
Health Minister Mark Butler describes the atrocious health outcomes, social exclusion and widespread homelessness as ‘a shocking reflection on our community’. The situation is revealed in a report by The Australian and Australian National University.

The plight of those with severe mental illness is “a stain on our nation”, according to federal Health Minister Mark Butler who has described the findings of a new study into the decades-long neglect of those with complex needs as “a shocking reflection on our community”.
The Australian National University report, compiled in partnership with The Australian, contains groundbreaking health economics analysis of the unmet needs in mental health care, housing and social services, and is augmented with empirical reporting and human stories told at the frontlines of the nation’s mental health crisis.
The report, titled Don’t Walk By: Unmet Need in Chronic Severe Mental Health Conditions, finds that government spending on mental health-related services is as low as about 7 per cent of total government health expenditure, despite mental ill-health accounting for the nation’s second-biggest burden of disease next to cancer.
The Productivity Commission has estimated that on a conservative basis, mental illness is costing the nation around $200bn to $220bn a year – just more than a tenth of the size of Australia’s entire economic production.
“Despite this enormous expenditure there is evidence that a substantial proportion of people with the most chronic severe mental health conditions – schizophrenia, bipolar disorder and severe depressive disorders – do not receive adequate care, if they receive care at all,” concludes the ANU/The Australian report, authored by psychiatrist Jeffrey Looi, professor of medicine Steve Robson, and with empirical reporting contributed by Natasha Robinson, the author of this article.
Responding to revelations in the report that Australian hospitals are short more than 10,000 mental health beds, and as many as 230,000 people with the most severe forms of mental illness receive no housing or social supports, Mr Butler said the nation must do better.
“The predicament of people with severe chronic mental illness has been a pretty shocking reflection on our community, as long as I can remember,” Mr Butler said. “I think it’s a stain on our nation.
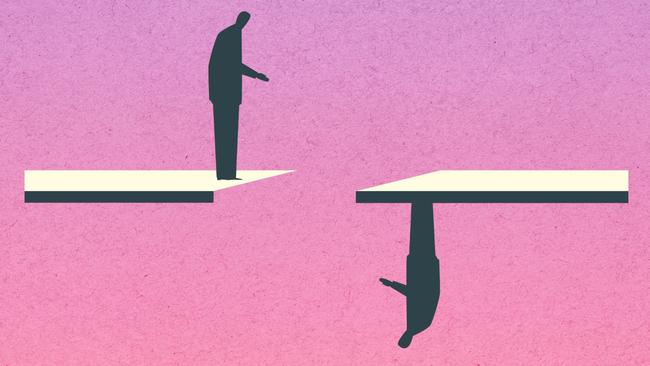
“I think at different steps in the journey from the Burdekin report and along the journey of deinstitutionalisation, the intention of which was all very well intended, it was not followed up with community investment. That has meant that for nearly 30 years, despite good intentions and periods of strong investment, that community, probably around 1 per cent of the population, has experienced enormous social exclusion, terrible life expectancy and health outcomes, very poor employment, massive over-representation in homelessness and prison populations, and we’ve got to do better.”
The 1993 Burdekin report into human rights and mental illness is regarded as a watershed in the move to shift mentally ill people out of institutional care and into the community.
The ANU-The Australian policy report found that the nation’s hospitals have fewer than half the psychiatric inpatient beds needed and billions of taxpayer dollars are being wasted through the failure to provide secure housing to those with complex needs. However, it says that simply providing more hospital beds is not the answer. If supported assisted accommodation wrapping healthcare and social supports around secure housing were provided to those with severe mental illness, it would slash the need for inpatient psychiatric beds by as much as 75 per cent, it says.
The ANU/The Australian policy report is the nation’s first comprehensive economic analysis of the extent of the monumental unmet need in severe mental illness across the spectrum of frontline healthcare as well as social supports, and reveals a vast tide of suffering at a huge cost to the nation. The cost of the shortfall in the provision of healthcare, social services and housing for those with severe mental illness amounts to around $8bn a year.
The report finds that Australia needs 17,750 psychiatric inpatient beds to meet current demand, but provides only 7000. The shortfall of 10,750 beds a year that is required would cost taxpayers $4.7bn a year.
And there is a shortfall of 31,000 housing places nationally for the severely mentally ill. A national spend of $5bn annually on housing could slash the number of psychiatric inpatient beds required by as much as 75 per cent.
A recent government analysis of unmet need in the provision of psychosocial supports for those with severe mental illness presented to commonwealth and state health ministers found 230,000 receive no psychosocial supports whatsoever. In total, 647,000 Australians with severe or moderate mental illness are not getting adequate support.
Previous existing state programs were rolled into the National Disability Insurance Scheme upon its formation five years ago, and the estimated three-quarters of those with severe mental illness who are not eligible for the NDIS were locked out of accessing any supports.
“That is a very big group of people who are getting no support, either through the NDIS or the other remaining programs at state level,” Mr Butler said.
“We know now it’s a really big group, much bigger than we knew and bigger than the estimates compiled previously by the Productivity Commission.
“This is something that’s sort of outside the strict remit of health ministers, but just reaffirms that these issues go well beyond clinical into a whole range of other areas – employment, housing, education. As we as health ministers start to come to grips with that, this report just highlights again how broad the response to this unmet demand needs to be.”
Mental health: Cast Adrift

Home truths: jails overflow as mentally ill live on the streets
Since the closure of mental asylums, the ranks of prisoners and the homeless have swelled with the severely mentally ill.

‘Nowhere to go’: supported housing could ease the burden of mental illness
Investments in housing for those with severe mental illness would reap enormous gains and savings for the nation.

Shocking plight of mentally ill ‘a stain on nation’
Health Minister Mark Butler describes the atrocious health outcomes, social exclusion and widespread homelessness as ‘a shocking reflection on our community’. The situation is revealed in a report by The Australian and Australian National University.

The clearing out of asylums was meant to provide hope. Instead it spawned an underclass
The severely mentally ill were promised a better future after asylums were mothballed. The promises were hollow.

‘My nightmare of trauma and terror’
I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system. This is my story.
Shocking life expectancy gap has not shifted in a century
The huge gap in life expectancy between those with severe mental illness and the rest of the population is growing in Australia, with no improvement in sight.

‘As a father I’m heartbroken, as a taxpayer I’m appalled’
Patrick Leunig went to a top private school and was set to study law. Then his life spiralled downwards. His grief-stricken father tells of how our system failed his son.

Freedom fight: Locked up and invisible in the heart of Australia
A young Aboriginal man’s escape from hell charts a community win for one of the many cognitively impaired and mentally troubled First Nations offenders who languish in our prison system.

Australia has a chance to fix its mental health system. Will we take it?
Australia’s broken mental health system has failed hundreds of thousands of people with severe illness with ineffective care – and that’s if they can access any at all. But one initiative may shift the dial.

‘The mental health ward became my prison cell’: a patient’s plea for change
Billie spent more than 1000 days in hospital before she turned 18. Damaged but determined, she is now speaking out for mental health reform.
Mr Butler has asked commonwealth officials to examine the psychosocial unmet needs report compiled by a joint commonwealth-state working group of senior bureaucrats and will present their analysis at the next national meeting of health ministers early next year, likely early February.
“Having this new (ANU) analysis as we do that is a really valuable contribution,” Mr Butler said.
“This year has been a time where community awareness of this issue has really been heightened by the tragedy at Bondi Junction and by the advocacy of a lot of people who were impacted by that tragedy, and the sector itself. There’s a lot happening in the space.
“We know from past examples of programs that have worked for people with severe and chronic mental illness (that) they have to be holistic, they have to be cross-portfolio, and they have to be joined up.
“The thing in my mind, which we were thinking about at the last meeting of health ministers, was the degree to which the physical health needs of people with severe and chronic mental illness often just fall off the edge of the table, because their mental health needs can be so profound.
“This is just not a new insight. This has been a real disparity in equity in our community for a very, very long time.”


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout