How Haven Foundation is providing hope to Aussies with psychosocial disabilities
The Haven model has proved not only life-changing for residents with complex mental health conditions, it also results in efficiencies for the NDIS and the health system as a whole.

Life has never been better for 42-year-old Sheree Barton. The Melbourne woman experienced years of insecure housing before moving into a private apartment within a supported living home in the western suburb of Laverton built by the Haven Foundation, a charity that is a subsidiary of mental health service provider Mind Australia.
The residence contains about 16 private apartments, each of which has its own kitchen, living room, bathroom, laundry facilities and outdoor area, built around beautiful gardens and a shared living area with a large communal kitchen that opens out onto a large backyard.
Having her own permanent residence with 24-hour support from health and social workers has transformed Ms Barton’s life.
“I walked in here for the first time and I just thought: ‘this is my home’,” Ms Barton says. “My health has improved. My mental health is fantastic now. I was getting sick all the time before, but now my health is just really stable.
“I take my medication, go to appointments, I work with the staff here on my goals, and communicate a lot with them. If I’m hearing voices, I speak up. I’m pretty aware now. I’ve got a lot of insight. I know when I’m getting unwell. I’ve got my tool kit – I listen to music, go for a walk, do some cooking. And the staff are available all the time.”

Ms Barton takes enormous pride in her apartment. She has decorated it beautifully, her shelves stacked with plants, vases and candles, and the couch draped in a favourite pink blanket.
The Haven Foundation was formed in 2006 by a group of families, friends and carers of people with mental ill-health. It now has 10 long-term housing residences for people with psychosocial disability in Melbourne and regional Victoria, and has 17 more under way. Three of the homes under construction are in NSW, and one is being built in Adelaide.
Secure housing is recognised as a key pillar for recovery from mental ill-health, and having health and social care provided in-house is crucial for people such as Sheree, who live with trauma from past experiences, not least in the mental health system.
“It was hard before I moved here, I was struggling to cope,” Ms Barton says.
“I had to rebuild my life again. I’ve had good times and bad times. The experience of being a patient is pretty scary. People are violent, they’re yelling and screaming. It was traumatising.”
The Haven model operates like a co-operative, where residents contribute a portion of their NDIS core funding to the Mind Foundation, which then delivers 24/7 shared support to residents. The support can be one-on-one, based on need. Support provided to residents includes help with the activities of daily living, personal care, medication management, budgeting, community access and peer support.
“If I’m hearing voices, I speak up. I’m pretty aware now. I’ve got a lot of insight. I know when I’m getting unwell. I’ve got my tool kit – I listen to music, go for a walk, do some cooking. And the staff are available all the time.”
Residents pay 30 per cent of their disability support pension plus their Commonwealth rent assistance towards their own rent. It’s a far cry from the private supported boarding house market, which emerged after the closure of long-term mental hospitals. Many residents in those boarding houses, some of which operate well, while others are places of squalor, pay between 75 and 95 per cent of their pension to landlords, and receive minimal support other than medication management and daily cleaning of bedrooms. Such a market has flourished because there is simply nowhere else for many with chronic severe mental health conditions to go.
Mental health: Cast Adrift

Home truths: jails overflow as mentally ill live on the streets
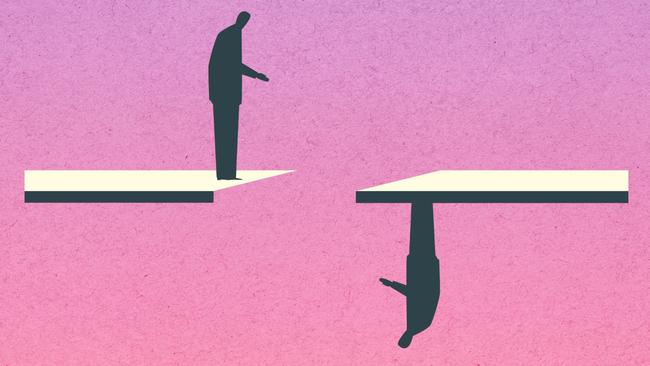
Since the closure of mental asylums, the ranks of prisoners and the homeless have swelled with the severely mentally ill.

‘Nowhere to go’: supported housing could ease the burden of mental illness
Investments in housing for those with severe mental illness would reap enormous gains and savings for the nation.

Shocking plight of mentally ill ‘a stain on nation’
Health Minister Mark Butler describes the atrocious health outcomes, social exclusion and widespread homelessness as ‘a shocking reflection on our community’. The situation is revealed in a report by The Australian and Australian National University.

The clearing out of asylums was meant to provide hope. Instead it spawned an underclass
The severely mentally ill were promised a better future after asylums were mothballed. The promises were hollow.

‘My nightmare of trauma and terror’
I am a 29-year-old woman living with treatment-resistant schizophrenia. I spent most of my younger years in and out of the public mental health system. This is my story.
Shocking life expectancy gap has not shifted in a century
The huge gap in life expectancy between those with severe mental illness and the rest of the population is growing in Australia, with no improvement in sight.

‘As a father I’m heartbroken, as a taxpayer I’m appalled’
Patrick Leunig went to a top private school and was set to study law. Then his life spiralled downwards. His grief-stricken father tells of how our system failed his son.

Freedom fight: Locked up and invisible in the heart of Australia
A young Aboriginal man’s escape from hell charts a community win for one of the many cognitively impaired and mentally troubled First Nations offenders who languish in our prison system.

Australia has a chance to fix its mental health system. Will we take it?
Australia’s broken mental health system has failed hundreds of thousands of people with severe illness with ineffective care – and that’s if they can access any at all. But one initiative may shift the dial.

‘The mental health ward became my prison cell’: a patient’s plea for change
Billie spent more than 1000 days in hospital before she turned 18. Damaged but determined, she is now speaking out for mental health reform.
The Haven model has proved not only life-changing for residents, it also results in efficiencies for the NDIS and the health system as a whole. A Haven home for an NDIS participant is less than half the cost per year of the national average cost of housing for an NDIS participant in supported independent living. The average healthcare costs for a resident in the Haven model is a little over $200 a day per person, compared to a cost to taxpayers of $1300 a day for a public mental health hospital inpatient.
Now that her health is on a positive trajectory, Ms Barton has been able to focus on gaining greater independence. She has been volunteering at Vinnies, and has just started a paid position there two days a week. It gives her some precious spending money to indulge one of her hobbies – purchasing fashion items.
“One of my goals is working on budgeting,” she says. “I’m getting some money, getting new skills, meeting new people. I’m a lot happier now.”


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout