What women need to know to support the men in their lives
After producing a guide to women’s health for the men in their lives, our expert GP columnist offers a baseline look at male health for mothers, wives, sisters and female friends.

Many men don’t think they need to see a doctor when they have no symptoms. Social norms can make them feel that seeking health guidance is not masculine. Or they may want to avoid an embarrassing examination.
And so sometimes it falls to the women in their life to encourage men to get the necessary checks and take the basic steps needed to stay healthy. Here’s what mothers, sisters, wives and friends should watch out for.
Childhood
Trauma, accidents at home
If we take a life-course approach and start from childhood, home is where most injuries occur and is responsible for 45 per cent of preventable death and injury in childhood. Boys have higher rates than girls of death or serious injury from accidents because of the socialisation process that leads males, from the time they are very young children, to engage in riskier behaviour than females, and to be supervised less by someone who might protect them from risk. It seems obvious enough, but never assume that a swimming pool or a toy is safe. Keep chemicals and household cleaners out of reach in locked cupboards; keep your medicines sealed and in a cupboard your young children cannot access. If poisoning has occurred, know to contact the Poisons Information Centre on 131126. I also recommend not leaving your children alone with food; when my son was four, he choked on a piece of broccoli that failed to dislodge with all the usual efforts, so I held him upside down by the legs, slapped his back firmly, then inserted a finger to the back of his throat and scraped hold of the leaf that was still attached to the stalk and small broccoli piece. Fortunately I was there, preparing our dinner, but it remains an unforgettable scene and reflecting on the “what if” fills me with horror to this day.
Undescended testes
In infancy, the routine post-delivery check of any male baby includes confirmation that the testes, colloquially referred to as balls, have descended into the scrotum (the skin sac that houses the balls). The development of testes, which also are referred to as gonads, the collective term used when referring to testes and ovaries, occurs in the abdomen in the fetus, and in males the testes descend into the scrotum before birth.
About 3 per cent of the time they remain in the abdomen or get stuck in the inguinal canal (groin) on their way down, a condition also referred to as cryptorchidism, a Greek term meaning “hidden testicles”. This should be corrected surgically by the age of two to fix the testicles into the scrotum using a procedure called orchidopexy, as there is a much higher risk of testicular cancer and long-term reduced fertility occurring in these males from teens onwards. Nappy change provides an opportunity to check that testes are where they should be and that they don’t retract into the groin.
Inguinal hernia
The journey of the testes to the scrotum through a natural channel in the abdominal wall called the inguinal canal remains an anatomical weak spot in males and is the reason an inguinal hernia, which can appear as a lump on the groin with exertion, is up to 10 times likelier to occur in men than in women. The bulge in the groin or lower abdomen is often painless and reducible and in some can even extend into the scrotum. In most men they will require surgical treatment eventually, which involves a day procedure and often the insertion of mesh, to strengthen the weakness in the abdominal wall.
Adolescence and young adulthood
Testicular cancer
Cancer of the testes is not that common, with just more than 1000 cases a year, but it affects mainly young men and is highly treatable when caught early. Basically, there are two types of testicular cancer: the non-seminoma group, which are more common in teens to mid-20s, and the seminoma group, which occur in 25 to 45-year-olds, although both can occur in any age group.
Encouraging young men to self-examine for scrotal lumps might be difficult for a mother to bring up in conversation but should be raised especially if there is a history of undescended testes, family history, previous testicular cancer, anatomical variations of the external genitalia where the urethra (the hole you pee from) opens underneath the penis.
Fortunately for cricketers, footy, rugby players and others involved in contact sports, there is no correlation between previous injury to the balls and cancer risk. Self-examination should be encouraged as a routine part of good preventive health in men at all ages. It involves having a feel around their testes especially when in the shower and rolling the testicles between each finger to feel for lumps, pain, hardness or irregularity in shape and size. If a lump, tenderness, or a hard testicle are detected, men should see their GP, who can arrange an ultrasound and referral to a urologist. Generally, needle biopsies are not performed with testicular lumps, as cancer cells from these can travel.
Acne
As boys enter puberty and adolescence, hormones surge, resulting in the obvious growth spurts, facial hair, pubic hair in armpits and groin, and increased body hair on the chest and legs. The voice deepens, an Adam’s apple will appear, and some may develop acne on their face and back that can be quite severe and can affect self-confidence. Acne should be attended to by the GP rather than with over-the-counter measures in the first instance and, if a positive response is not achieved, a referral to a dermatologist should follow for the start of medication that can prevent irreversible scarring and psychological consequences. It is a time when boys can feel awkward about a variety of things, similar to adolescent girls, who also experience concerns about body changes.
Gynaecomastia
Another common result of hormonal surges is gynaecomastia, which is the appearance of breast buds and occurs in up to 50 per cent of boys. This happens when sport and showering in change rooms with other boys can cause enormous embarrassment. Let them know it is not serious but a normal hormonal consequence of circulating oestrogen (the female hormone), and this will level off after age 16, as will the breast tissue. Reassure them if there is pain, as this is normal too, and if breast tissue persists for more than three years it can be treated medically or even surgically. This is also a time to encourage sun-smart behaviours as the risk of malignant melanoma in Australia continues to climb despite the “slip slop slap” campaigns. Recommend hats, sun block, sunglasses and rash tops. Avoid peak UV exposure.
Family relationships

Many mothers who see me lament that their boys who were once close and affectionate have become distant, avoid cuddles and are virtually monosyllabic in their responses to questions. It’s difficult to get to the bottom of what is changing, but in Stephen Biddulph’s book on raising boys he talks about the need for the adolescent male to spend time with positive male role models, elders, fathers. It’s not always as easy as just making that switch if the father is absent, travelling or working long hours.
Father-son time is something the parental unit will need to negotiate even where there is a division of the household between two places. For those who are sports-oriented, this is often the lever that enhances opportunities for positive experiences for both son and father. For those who are less sporty, activities such as scouts, camping or building something together can provide the annex to life outside and away from the influence of social media. Where there are father-son tensions, being around other father-son groups is a good place to engage, break the ice and build a healthier relationship.
Social media
It has been said that the most dangerous place for an adolescent male is alone in his room, and there is evidence that checking social media repeatedly in young teens changes their brain development in as little as three years. If a teenager accesses their social media more than 15 times a day, it will generally make them more prone to anxiety and emotional sensitivity in social settings.
Most parents have found themselves out of their depth in knowing how much screen time is acceptable, especially when so much learning is online. The adolescent brain is vulnerable to forming patterns of behaviour from neural pathways that are being formed for years to come, which means it is worth letting the adolescent know that limiting use is better for brain development and mental health. Try to get boys outside and physically active, even if it means you or their father goes with them.
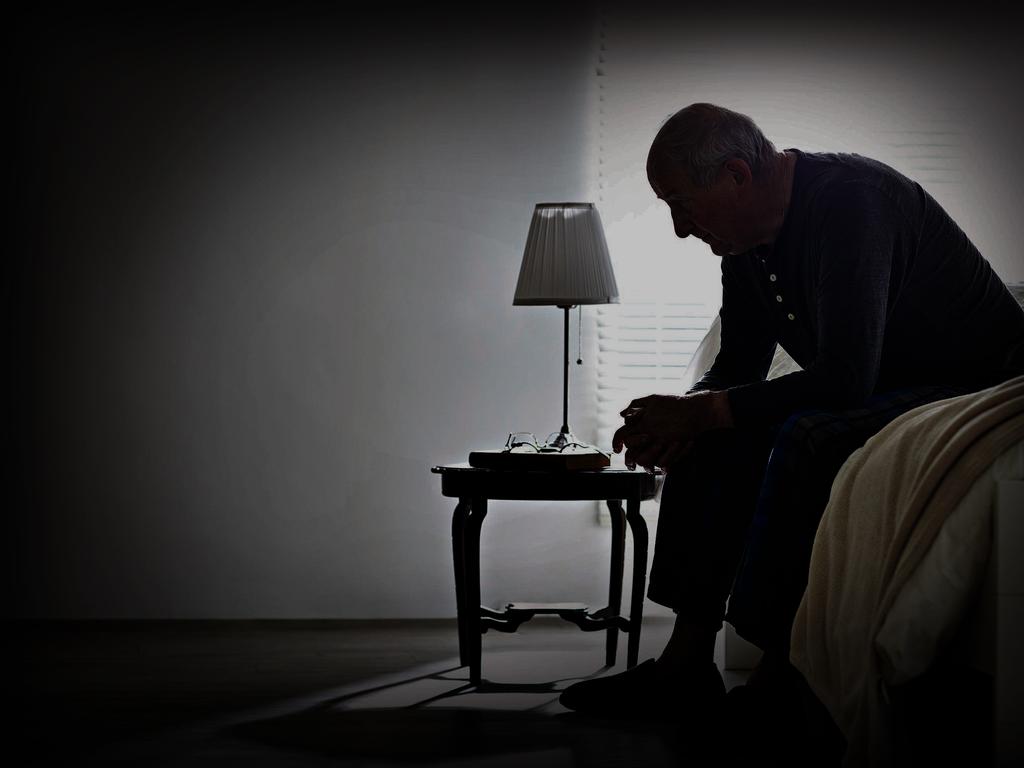
Mental health
Up to 50 per cent of mental health issues present in adolescence in males and although the severe 15 per cent of these eventually will be identified and treated, the 70 per cent with moderate anxiety and depressive disorders remain unmanaged and can continue through to adult years.
Of major concern is that severe depression is not always a precursor to suicide and a young man may end his life impulsively, without warning, while under the influence of alcohol, drugs or during other risk-taking behaviour. Maladaptive behaviours such as these increase in likelihood around adolescence especially where there is family dysfunction or learning difficulties or bullying at school.
The consequences of adolescent loneliness and isolation, and family or peer-group dysfunction are a national tragedy, with suicide being the commonest cause of death from ages 18 to 45. Our schoolteachers are overwhelmed by the prevalence of adolescents who have mental health issues, and much can be said about the impacts of social media on young men’s minds (as with young women).
Social media can contribute to loneliness and self-doubt, and adolescents can be drawn into echo chambers of competitive noise that erode self-confidence, limit in-person communication and distort thinking around relationships. Once upon a time, bullying and harassment were more visible and occurred in the schoolyard where teachers could intervene; the online version, however, is invisible, shrouded in silence, and can be even more pervasive.
Pornography
You should talk to your sons about online pornography; it is harmful, toxic and mainly portrays and condones sexual behaviours where there is violence against women. A paper by the Australian Institute of Family Studies (AIFS 2016) revealed that by age 12 about 50 per cent had seen pornography and by 17 years 75 per cent had. More recently, the Our Watch survey found one in three adolescent boys surveyed had accessed “violent and degrading pornography” to teach them about sex.
If we consider that the brain is creating neural pathways for behaviours in adolescence and that these can become fixed, the concern is that this is learned and acted out in relationships, which puts young men in the precarious position of being an aggressor, not a lover, with disastrous personal, relationship and social impacts. In short, what young men see in online pornography, is not reflective of respectful relationships, yet it is what they are learning from. This needs to be addressed at home as much as it does at schools and through national campaigns such as Consent Can’t Wait, which talks about respectful relationships and consent.
Middle adulthood and beyond
Preventive checks
In general, men see doctors less often than women around the same ages, mostly because women will have several reasons to see the GP with issues related to menstruation, contraception, gynaecological screens and pregnancy, which provide opportunities for preventive health discussions.
Men don’t have these biological reasons to attend so generally will visit for an injury or other acute problem such as an infection or a repeat prescription, and consequently the opportunistic, preventive health discussions occur less frequently.

Unintentional neglect of personal health is associated with low health literacy, even in men with professional qualifications, and when they do present, their disease is usually more progressed. The best advice you could give a man of any age is to have an annual health check with a general practitioner.
Keep in mind that social isolation and loneliness are each risk factors for poor physical and mental health, suicide and chronic disease. The Royal Australian College of General Practitioners Red Book is our national general practice guide for preventive health checks in Australia. It recommends that heart disease and diabetes screening start at age 40 for the bulk of the population, and specific 40-plus and 45 to 49-year-old health checks can each be performed once to get a baseline and provide lifestyle advice. These are fully reimbursed by Medicare.
Men generally won’t talk voluntarily about what’s going on emotionally in their life and they mostly keep what they’re feeling to themselves. Reading body language and being a good listener is a very good place to start, so where there are concerns about their mental health or things just don’t seem right, ask how they are coping or feeling.
In one of my earlier articles on men’s mental health, a common response was “I want to talk but no one is listening”. When chatting, ask what’s good about things and what’s not good. A lot of stress can result from issues at work, but relationship breakdown is also a trigger for increased alcohol consumption, social withdrawal, drug taking, risky behaviour and feelings of despair. In my first article on men’s mental health, I point to resources that can provide some help, but just listening and being empathetic can make a big difference to how they feel.
Lifestyle, chronic disease prevention
Men have a life expectancy of 80.7 years, which is lower than women at 84.9 years. The leading cause of death for men is coronary heart disease, followed by lung cancer and dementia including Alzheimer’s disease. These statistics are improving gradually, but the farther away from a metropolitan region a man lives, the likelier he is to have health risks and suffer chronic conditions than those who live in cities, so if you have a dad, a brother or cousin out there, weave some questions around health into the conversation and ask if they have a GP. Where they don’t have one, recommend they get one, and if it’s too hard invite them to see yours.
Knowing family history of chronic diseases such as diabetes, heart disease, blood pressure stroke and cancer is important, as this identifies increased risks that are genetic and lifestyle related. Having a first-degree relative (mother, father, brother, sister) who has had heart disease before the age of 60 increases the risk of heart disease significantly. Make sure he knows his family history so this can guide your conversations on getting a fasting cholesterol, sugar, blood pressure and weight check.
Even where there is a genetic tendency, the risk of disease can be reduced when lifestyle modifications are started early, and the mid-30s is a great time to start thinking about this.
The checklist below remains the same for blood pressure, diabetes and even dementia. It’s just all-round good advice and you can give this to just about anyone without ever worrying whether your information is incorrect.
Prostate cancer
Cancer of the prostate is the second-most diagnosed cancer and the second-most common cause of cancer death in Australian men. Although advice around this varies according to where you get information, my recommendation is that getting a baseline prostate specific antigen (PSA) blood test from the age of around 50 is a good idea. If there is a first-degree relative with prostate cancer younger than 65 years, this should start earlier, at 45.
A higher PSA reading does not always mean cancer and a normal reading may miss a cancer as symptoms can be silent, but at least it opens the conversation. Although overdiagnosis is a concern, the risks and benefits of further investigations can be discussed.
Bowel cancer
Bowel cancer screens are easy and should be done from the age of 45 now. For those who have avoided acting on the government bowel cancer test kits sent to them in the mail, I request that they enter the words “order poo test” into the browser on their phone, scroll down to the National Bowel Cancer screening link and click on “order test kit”. I do this in my rooms with my patients often, especially with the ones who cringe at the thought of dipping a cotton tip into their excrement over three days, which is basically what is required. I explain graphically that bowel cancer can be silent and deadly but is most preventable if caught early. Then I follow up that this has been done. Easy.
Osteoporosis
A government-subsidised bone-density screen is recommended for men at the age of 70 and for all Australians who have not had one before, as a baseline. Although most think it is a disease only of post-menopausal women, a quarter of sufferers are men, so recommending this test to your partner, father, brother, after you have been advised to have this yourself, can get more men thinking about bone health. For older men, it can be linked with other preventive activities such as vaccination for pneumonia, shingles, influenza, whooping cough, Covid and RSV.
Although this is not a complete list of key health issues for men, women do tend to be the ones who prompt the males in their life to visit doctors. Hopefully, raising awareness this way can instigate more of these conversations and bring men in to see their general practitioner before preventable, advanced disease occurs.
Magdalena Simonis is a GP, RACGP Red Book reviewer and clinical associate professor in the department of general practice, University of Melbourne.
This column is published for information purposes only. It is not intended to be used as medical advice and should not be relied on as a substitute for independent professional advice about your personal health or a medical condition from your doctor or other qualified health professional.
References
- Why Men Avoid Doctors
- Injuries in Children and Adolescents
- Guidelines for preventive activities in general practice
- Australian Family Physician Vol. 32, No. 6, June 2003 Robert H Hall
- Parent MC, Gobble TD, Rochlen A. Social Media Behaviour, Toxic Masculinity, and Depression. Psychos Men Masc. 2019 Jul; 20(3): 277-287. doi: 10.1037/men0000156. Epub 2018 Apr 23. PAID: 38250140; PMCID: PMC10798810.
- Children and Young People’s Exposure to Pornography
- Respect
- Pornography As Sex Education
- Heart Foundation
Resources
- Biddulph Steve: Raising Boys In The Twenty-First Century
- How To Help Our Boys Become Open-Hearted, Kind And Strong Men
- Consent Can’t Wait





Back in 2003 an article in the GPs’ journal Australian Family Physician urged doctors to tell women about male health “because men seek health information from doctors less frequently than women”, and on that score little has changed.