We hear a lot about women’s health. Here’s the essential guide for dads, partners, friends
As a father, brother, partner or workmate, you want to understand some of the basics about the health of the women in your life. Here’s some practical information that will help.

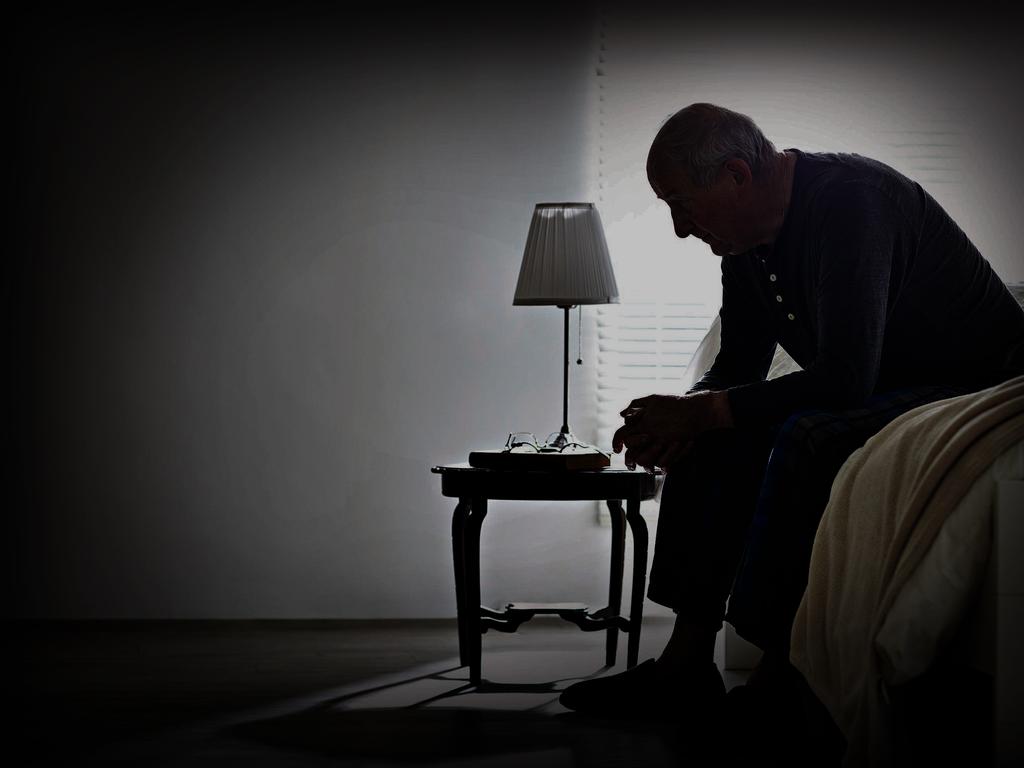
As a father, partner, brother, work colleague, friend, there will be women in your life whom you care about. With the array of issues being discussed in the media on women’s health – ranging from heavy menstrual bleeding, endometriosis, pelvic pain and menopause – it can all seem quite far removed from you, and switching off from it all would be totally understandable.
This article aims to demystify “women’s business” in the hope that some of the challenges women face and the attention these conditions are receiving can be explained. This piece will be followed by a subsequent article, which will cover what women should know about men’s health, to better support their sons, brothers, partners and friends.
From puberty to menopause
Knowing the basics about periods – such as what’s normal and what’s not, how to help as a father or partner, or how to provide support – is important for men who live with or work with women. Females will have periods that usually start about 18 months after the onset of puberty and recur for at least 40 years over their life.
For those of you who have daughters, you will observe obvious physical changes appearing anywhere from nine to 13 years of age. Aside from these, there can be emotional fluctuations too. Puberty that begins before nine years of age is considered early and if there are no signs by 13, then it is late; both fall outside the normal range and should be investigated. There will be the development of breast buds, pubic hair, some facial acne, often some stretch marks and the onset of menstrual bleeding, most of which will cause your daughter embarrassment and hypersensitivity around the way her body looks.
Teenagers are vulnerable during this phase, as they face enormous pressure from peers and social media influencers that flood their followers with unrealistic images of blemish-free skin and lean bodies. As many already feel uncomfortable with their bodily changes, it’s unsurprising that up to 50 per cent of mental health disorders develop in adolescence.
There’ll also be additional shopping items on your list such as sanitary napkins and tampons and a mix of ibuprofen or paracetamol for cramps and headaches that might be associated with the first days of the menstrual flow.
Be aware that pain that isn’t relieved with simple, over-the-counter medication and a hot water bottle, or that stops your daughter or partner from doing day-to-day things, is abnormal and should be investigated.
Not all girls and women suffer mood swings in relation to their periods – commonly referred to as “premenstrual syndrome” (PMS) – but if they occur, they’re usually alleviated with the onset of bleeding. There might be tears with little provocation (dad jokes fall like lead balloons), breast tenderness, bloating and pimply flare-ups in the days before the period comes. All of this is driven by hormonal fluctuations.
In some, the mood swings can be very severe, and you might notice your daughter has angry outbursts and feels depressed for days to even up to two weeks before her period. This degree of disturbance crosses over into the category of Pre-menstrual Dysphoric Disorder (PMDD) and occurs in 3 to 8 per cent of women. This is a depressive illness caused by naturally occurring hormonal fluctuations that bring on a period. Some women are particularly sensitive to the hormonal ups and downs, and this triggers changes in the neurotransmitters in the brain such as serotonin and dopamine, which cause low mood and behaviour change.
It’s not likely your daughter will come to you for advice about any of this, but you will notice that things are different. If you are a single parent, or you and your ex-partner co-parent, it’ll help to know a bit about this so that you can support your daughter.
Pre-menstrual Dysphoric Disorder is often treated with oral contraceptives which regulate the hormonal highs and lows, so try not to overreact if you find that your 15-year-old has started taking the pill. Some might even need continuous or intermittent doses of mood-stabilising antidepressant medication. Over-the-counter remedies and high-dose vitamins have failed randomised controlled testing so a visit to the GP is recommended given the length of a woman’s reproductive lifespan and the cost to her and society of time lost from school, sport, work and life. It might be a particularly tricky time at home for everyone, especially if your partner is going through the perimenopause or menopause and suffering similar symptoms due to the naturally occurring hormonal fluctuations associated with age-related decline in ovarian function.
Much has been said on the topic of perimenopause and menopause and in my recent piece, which cuts through the hype, I provide some useful information. In a nutshell, about 50 per cent of women will have bothersome symptoms at the tail end of their reproductive life, which usually occurs anywhere from 45 to 55 years of age. For most women, the symptoms are manageable and will resolve over six to 24 months with minimal or no intervention. Around 10 per cent will need ongoing menopausal hormonal therapy for some portion of their life.
Periods: what’s not normal

In the first few years of adolescence, periods can be all over the place. There can be months of no periods followed by a few regular cycles. This usually normalises and a predictable pattern ranging from 21 days to 35 days is finally achieved around late teens. If periods remain irregular after that, there is a high likelihood your daughter is at risk of having polycystic ovarian syndrome or PCOS. This is one of the commonest hormone disorders affecting up to 12 per cent of women during their reproductive life and is often associated with acne, easy weight gain, hirsutism (excess hair where you don’t want it), mood swings, the appearance of numerous cysts on ovaries (sometimes the cysts rupture, causing pain).
This condition predisposes her to reduced fertility, diabetes and high blood pressure in later life but can be managed by seeing a GP early on. In around half the PCOS sufferers, the mother will have had similar issues and may have had difficulties conceiving.
The GP will take a history, perform an examination, order baseline tests to check her hormone profile including male hormone levels which can be elevated, thyroid function, blood glucose and insulin levels. A pelvic ultrasound is often recommended but isn’t reliable as up to 70 per cent of teenage women have numerous ovarian cysts. At the review of all this, the discussion will be around the treatment options which may or may not include hormone therapy, often in the form of the oral contraceptive pill or metformin, a diabetes medication. The aim of prescribing the contraceptive pill is to regulate these hormones to create a 28-day cycle, which often also treats the acne and other related issues. A whole-of-lifestyle approach is necessary for this chronic hormonal condition, which includes exercise, eating foods with a low glycaemic index and treating the concerns she has regarding her skin and body changes.
At the other end of the spectrum, there are girls and women who have frequent or regular periods that last eight days or more, requiring a change of pad or tampon every couple of hours. It’s not uncommon to wake through the night with blood-soaked bedclothes and sheets. This degree of blood loss is abnormal even if there is minimal or no pain associated with it and is referred to as heavy menstrual bleeding. This affects around one in four women, of whom up to 50 per cent will develop endometriosis, which is the dreadful chronic inflammatory disease of the uterine lining, called the endometrium, which sheds each menstrual cycle but in some, refluxes through the fallopian tubes into the pelvis.
Endometriosis affects around one in nine women and if untreated can lead to internal pelvic organ damage, chronic pain, disruption to education and career, and even infertility, so it’s worth knowing what falls outside the range of normal.
As with PCOS, endometriosis has a strong genetic tendency so is 10 times more likely to develop in your daughter if her mother has had this condition. It’s very likely that you have been impacted directly too, if your wife has been curled up in tears with excruciating pain during and after her periods. Even being lightly touched can set off the pain that affects her bowels, back, bladder and destroys your sexual intimacy. The effects on your relationship can be devastating.

In addition to all this, heavy periods increase the risk of iron deficiency and anaemia, so if your teenage daughter is going through a vegetarian or vegan phase, the risk is even greater. Signs of anaemia include fatigue and having a low mood. Keep this in mind if she just doesn’t want to get up in the mornings. Certainly, being up late into the night on social media might be an additional culprit which could explain morning grumpiness and fatigue, but it isn’t always just that. If you share a love of sport with your daughter and coach her soccer or basketball team or take her to tennis, be aware that having good iron stores makes all the difference to energy levels and fitness, so it might be time to don the barbecue apron and bring out the tongs around four times per week.
Preconception counselling, miscarriage, pregnancy and the post-partum period
For any man who has been in a relationship with a woman and trying to conceive, a point is reached after months of negative outcomes when concern regarding fertility will have led you to the general practitioner’s office. Conversations these days go along the lines of “the ovulation tracker says”, and if the male partner attends, it’s “my partner says I need to have my sperm checked”.
Ideally, couples should see the GP for some preconception counselling before attempting to fall pregnant, but few ever attend for this. Most couples just launch into trying to conceive, with few knowing how important lifestyle changes are and how they improve the chances of conception, the health of sperm and even the health of the baby and mother over the course of the pregnancy.
The most important first steps for the couple are to eat healthily, stop smoking, stop alcohol and for the woman to commence taking a pregnancy supplement which contains at least 400mcg of folic acid, 150mcg of low-dose iodine and vitamin D.
Genetic screening is readily available now so you and your partner can explore having a genetic test, especially if there is a family history of a heritable disorder on either side.
In up to 30 per cent of infertile couples, the problem is with the sperm. Age affects sperm quality too, which means this declines with time. Smoking, drinking alcohol, taking certain medications, drugs, being overweight, overheating the genitals with tight underpants and keeping your laptop quite literally on your lap, or even having hot baths and showers, can reduce the quality of your sperm. Simple behavioural measures that correct all these can all improve your sperm quality. However, once conception occurs, it’s not always guaranteed to be smooth sailing to delivery.
Little can prepare a couple for the disappointment of miscarriage, which is the loss of the pregnancy within the first 20 weeks. One in five pregnancies will end in miscarriage and it is even more likely to occur, the older the mother. It’s heartbreaking and although you and your partner might rapidly return to normal life on the outside, because you haven’t had the chance to tell people that you were “expecting”, the grief often persists. Seeing your GP to talk about this can help you both navigate the feelings of loss.
When a pregnancy continues successfully, your partner will be screened for depression as a routine part of the antenatal check and again after the baby is born. This is because women who have had previous mental health disorders are more prone to depression that develops during pregnancy. Ten to 15 per cent of women will be diagnosed with depression during pregnancy and if it appears within weeks of the delivery into the first 12 months, this is classified as post-natal depression.
The first step is to see the GP to talk about the changes at home. The GP will conduct an examination and some blood tests to rule out anaemia; they’ll address any sleep deprivation and maybe recommend a mother-baby sleep school to establish a routine. Counselling with a GP often suffices, especially when there is adequate support from the partner and network.
Medication can also be prescribed, even if the mother is breast feeding. After the delivery of the baby, those previously diagnosed with bipolar disorder are at a high risk of psychosis occurring for the first time, risking both mother and baby. This is a medical emergency, and you should call triple-0.
Coming home with a newborn baby is a happy time but also a time of immense change and it’s quite normal for you both to feel the need for some parenting support, as there are so many changes and babies can’t tell you what they need without crying. Your regular GP and maternal childcare nurse can help you, but for those difficult after-hours times, there is the Pregnancy, Birth and Baby video-call service which allows you to speak face-to-face with a maternal child health nurse 24/7. Parents often feel better with some reassurance from an expert. Another very useful online program I refer my patients to is the government Pregnancy, Birth and Baby website.
As outlined already, although men and women don’t share the same sex-related health issues, knowing how to respond when your loved one is in distress can make an enormous difference to her wellbeing and even yours.
References
- Premenstrual conditions
- Your Fertility
- Antenatal and postnatal depression
- Medicare Mental Health
- MumMoodBooster
- Mum Space
- Pregnancy, Birth & Baby
Dr Magdalena Simonis is a GP and associate professor at the University of Melbourne Department of General Practice.
This column is published for information purposes only. It is not intended to be used as medical advice and should not be relied on as a substitute for independent professional advice about your personal health or a medical condition from your doctor or other qualified health professional.



To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout