Christian was told nothing could be done to stop his prostate cancer. Now, it’s undetectable
Scientists ‘excited’ by promising trial results showing men with aggressive prostate cancer felt better and lived longer when taking a combined therapy.

Christian Edouard-Betsy was at work when his doctor called and asked him to meet immediately to discuss the results of a blood test for his prostate.
“When I got there he just said ‘I don’t like your result and I think you’ve got a real active and aggressive prostate cancer’, and hearing that word ‘cancer’ – that just knocked me,” the now 66-year-old father of four says.
Further testing confirmed those fears and Edouard-Betsy underwent somewhat successful surgery, but the cancer had spread to his lymph nodes requiring him to take hormone therapy to try to control it, which seemed to work for a while. At the time, he was under the care of a urologist and was trying to get an appointment with an oncologist, suggested to him by a friend.
Only later did he realise that, after putting his name on a waitlist for the oncologist, he had changed phone numbers, rendering him uncontactable. In the meantime, Edouard-Betsy says his prostate specific antigen levels rose rapidly and became “out of control”. Then came another devastating blow.
“The urologist said to me, ‘I’m sorry, there’s nothing we can do’, and I thought, what?”
In a panic, Edouard-Betsy contacted the oncologist again who said they had been trying to get in touch with him for the past year. Unlike his urologist, she offered alternative drugs, all of which ended up failing. Then she told him about a clinical trial that was about to begin and she thought he could make a good participant.
“I said, ‘Well, I have no choice, have I?’ It’s an aggressive cancer and you either go big or go home. So she put my name down and I am one of the first patients who went through the trial.”
The trial was specifically for patients with aggressive prostate cancer, known as castration-resistant prostate cancer, for which there are few treatment options.
“A lot of men get prostate cancer that never kills them; they have treatment for it and they’re fine,” explains Professor Louise Emmett, study chair and director of theranostics and nuclear medicine at St Vincent’s Hospital in Sydney.
But she says between 10 and 15 per cent of patients get metastatic prostate cancer, where the disease spreads beyond the prostate and it is those men who this trial was aimed at.
“A lot of those men, when they first get diagnosed, they go onto hormone treatment which controls it for a while but then it becomes what we call castrate-resistant. When something becomes castrate-resistant, they have about three years to live. And in the particular group of men that I was treating, they have about a 5 per cent five-year survival (rate),” she says.

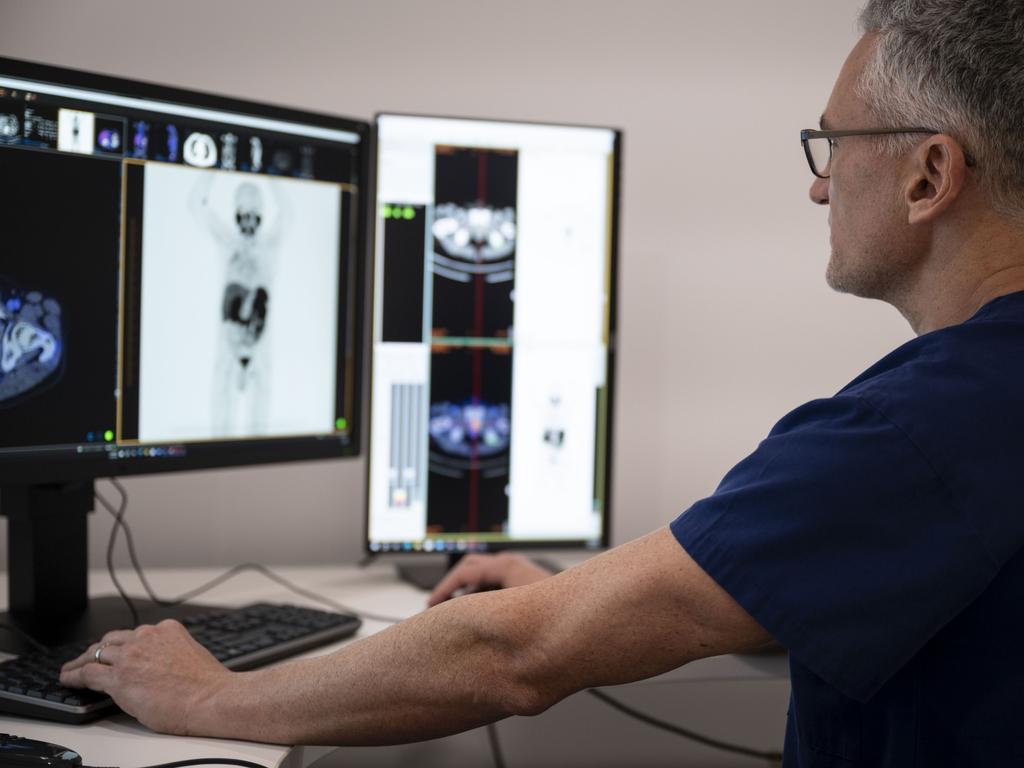
Emmett led the research team for what they called the ENZA-p study. One group was given the hormone drug Enzalutamide at a dose of 160mg daily, while the combination group was given the same medication as well as an adaptive dose, given intravenously, of Lu-PSMA-617 every six to eight weeks.
The open-label, randomised, phase 2 trial was carried out across 15 hospitals in Australia between August 220 and July 2022, though participants were then followed up on for many months after. It involved 160 patients, 79 were randomly assigned the hormone, while 83 were given the combined therapy.
After a median follow up of 34 months, 96 deaths were recorded. However of those who died, men in the combined group lived for a median of 34 months, compared to the first group where the survival median was 26 months.
Patients in the combination therapy group also reported having a higher quality of life because they were in less pain and were not as fatigued.
Emmett suggests the findings are exciting and suggests the therapy could even be used as a less toxic alternative to chemotherapy, though more studies are needed.
This work builds on previous studies of Lutetium-PSMA as a standalone therapy, with improvements to a patient’s quality of life. However, only a modest improvement in overall survival was seen with a median four-month benefit observed, and only in one study.
“It looks like these two agents together are super powerful. They’re more powerful together than they are on their own,” she says. “These are treatments that people get, that we usually give sequentially. So we do one, it fails, then we start the next. So what this does is it really raises the questions that we should be giving these treatments together, not only just in this space, but maybe even earlier. So we should be giving it to men who turn up with metastatic disease before they start failing treatments to try and stop the disease from getting hold and keeping it at low volume, and because it was so well tolerated.”
The findings are published in the medical journal The Lancet Oncology and are being presented by Emmett at the annual American Society of Clinical Oncology Genitourinary Cancers Symposium in the US.
“I’m excited by it because, for me, it’s a first step to finding something that really controls prostate cancer much, much better,” she says. “It’s non toxic, it works really well. What we need to do now is figure out where we use it: do we use it really early? Do we use it really late? Do we use second line hormone treatment? Do we use first line?
As it turns out, Edouard-Betsy was randomly assigned to be part of the combined therapy group and says his PSA levels went from “out of control” at the start of the trial to now being “undetectable”.

“I’m over the moon,” he beams while sitting next to Vicki, his wife of 40 years. “I was very emotionally happy about that and you get the shakes when you go through that. I still had one or two rounds to go (on the trial) and the professor said to me ‘we’re pretty sure you don’t need it, it seems to be working,’ and so I stopped early.”
He feels so much better he has even returned to the gym – something he had not been able to do in years.
However, while scientists here are leading the way with research in this area, there are still access issues with Lutetium-PSMA-617 in Australia. The drug is not rebated here and is only available to men in a clinical trial setting. However, the Medical Services Advisory Committee has recommended the drug be funded from July for men with late stages of the disease.
The study was led by the Australian and New Zealand Urogenital and Prostate Cancer Trials Group in collaboration between The Australian and New Zealand Urogenital and Prostate Cancer Trials Group, the NHMRC Clinical Trials Centre at the University of Sydney, and the Australasian Radiopharmaceutical Trials Network.
Prostate cancer is the most diagnosed cancer in Australia, with estimates of 26,400 cases and 3900 deaths last year alone. While the death rate is declining, the ageing population means cases are still rising. Health officials predict that by 2040 there will be 372,000 people living with prostate cancer in Australia.




To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout