Australia urged to take action in response to new mpox emergency
Australia has been urged to take action amid growing concern about “the most dangerous strain yet” of a deadly virus.

Health
Don't miss out on the headlines from Health. Followed categories will be added to My News.
Australia has been urged to step up its screening of travellers entering the country amid growing concern about “the most dangerous strain yet” of mpox, which health experts say is increasingly spreading via everyday touch rather than sexual contact.
The World Health Organization (WHO) on Wednesday declared the mpox surge in Africa a global public health emergency, sounding its highest possible alarm over the worsening situation.
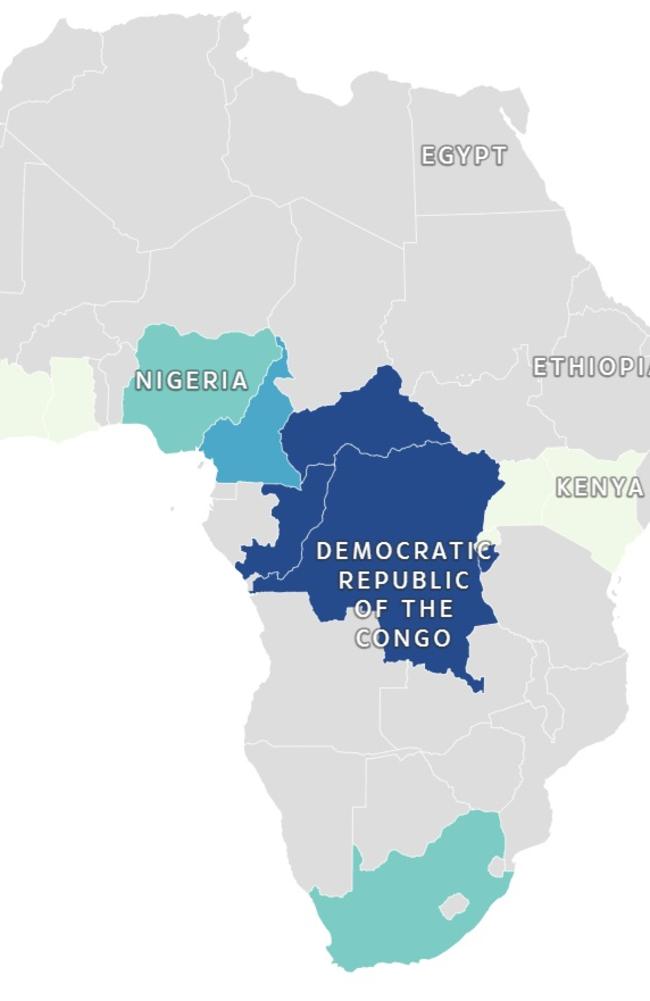
The more aggressive clade 1b strain of mpox, previously known as monkeypox, has now spread from the Democratic Republic of Congo (DRC) to 12 other countries across Africa including Burundi, the Central African Republic (CAR), Kenya and Rwanda.
The WHO hastily convened a meeting of experts to study the outbreak.
“Today, the emergency committee met and advised me that in its view, the situation constitutes a public health emergency of international concern,” WHO chief Tedros Adhanom Ghebreyesus told a press conference. “I have accepted that advice.”
A PHEIC is the highest level of alarm under the International Health Regulations, which are legally binding on 196 countries.
“The detection and rapid spread of a new clade of mpox in eastern DRC, its detection in neighbouring countries that had not previously reported mpox, and the potential for further spread within Africa and beyond is very worrying,” said Dr Tedros.
“It’s clear that a co-ordinated international response is essential to stop these outbreaks and save lives. This is something that should concern us all.”
The UN health agency’s decision comes the day after the African Union’s health watchdog declared its own public health emergency over the growing outbreak.
Dr Tedros said the more than 14,000 cases and 524 deaths reported so far this year in DR Congo had already exceeded last year’s total.
“The emergence last year and rapid spread of clade 1b in DRC, which appears to be spreading mainly through sexual networks, and its detection in countries neighbouring DRC is especially concerning,” he said.
More screening
Professor Robert Booy, infectious disease expert and chairman of the Immunisation Coalition, said Australia was in a “fortunate situation” and largely free from mpox, which is a close relative of smallpox.
“We have the fortunate situation in Australia where we have eradicated a number of diseases, obviously smallpox has been gone for over 40 years,” he said.
Mpox remains relatively rare in Australia but “it may come in [every now and then] on a plane”, he added.
Australia has detected only few hundred cases of mpox since the start of the last global outbreak in May 2022, largely affecting gay and bisexual men, with around 97,000 cases reported and 140 deaths worldwide.
Mpox is a viral infection with typically mild symptoms of fever, headache, muscle aches, swollen lymph nodes or fatigue, followed by a skin rash or lesions.
Victoria has been battling an ongoing outbreak with 108 cases notified so far this year, bringing the total to 190 since May 2022.
Queensland Health has recorded 22 cases so far this year, a spokesman said. NSW Health announced in June it had detected three new cases, bringing the total since May 2022 to 69.
Prof Booy said Australia already had “effective screening” through arrival questionnaire forms but that measures could be stepped up.
“We do check whether people have a fever or a rash but there may be a real benefit from being more focused and more specific about that checking on arrival,” he said.
The federal Health Department has been contacted for comment.
Mpox has emerged as a concern in Africa particularly among preschool and primary school children “as they tend to mix more closely”, according to Prof Booy.
“It’s generally not a deadly infection but in children who already have immunosuppression, malnutrition, HIV/AIDS, other serious conditions, it can become deadly so that’s why it’s of international concern,” he said. “What concerns [health authorities about the new strain] is that individually it can be severe and lead to overwhelming infection, and it also has potential to spread more easily, so those are the two things that always concern the WHO.”

Vaccines that help prevent against both smallpox and mpox are widely used in Africa and Prof Booy said Australia should chip in.
The WHO said it was working with countries and vaccine manufacturers on potential vaccine donations, as well as access to therapeutics, diagnostics and other tools.
“We already have a way of preventing it and we need to look closely as a responsible international country to work with the WHO to improve supply to those who really need it in those countries,” Prof Booy said.
But widespread vaccination in Australia was “certainly not needed” outside of at-risk groups, according to Prof Booy.
“All the different varieties of men who have sex with men, and sex workers too, whether male or female, should get themselves vaccinated,” he said.
In some cases travellers may also consider getting vaccinated.
“If you’re going to a country where it’s endemic or spreading and going to be living in the countryside, not a hotel, for more than one month, you have to think very seriously about measures that can be taken to mitigate and lessen your risk,” he said.
A Queensland Health spokesman said public health units in the state “continue to investigate new mpox cases as they arise, including contact tracing and identifying any epidemiological links”.
“Mpox does not spread easily between people and is mainly spread through very close or intimate contact with someone infected with mpox,” he said.
“People most at risk in Australia are gay, bisexual or other men who have sex with men. Vaccination is available for post-exposure prophylaxis as well as primary preventive vaccination.
“High-risk groups, including sex workers, are eligible for free vaccines through sexual health clinics and general practitioners. The government-funded mpox vaccine is available to people at greater risk of mpox infection through sexual health clinics and some GPs.”

‘Tip of the iceberg’
Dimie Ogoina, who chaired the WHO’s emergency committee, said the 15 members present unanimously thought the mpox upsurge was an extraordinary event.
He said many members feared the known situation in Africa was “actually the tip of the iceberg”, because without more robust surveillance, “we don’t have the full picture”.
Maria Van Kerkhove, the WHO’s epidemic and pandemic preparedness and prevention director, insisted, “We can stop transmission of mpox with a concerted effort.”
But she said experts needed a “much better understanding of the epidemiology” and the transmission patterns, which would help make sure the limited number of vaccines could be deployed to best effect.
Committee Chair Professor Dimie Ogoina said, “The current upsurge of mpox in parts of Africa, along with the spread of a new sexually transmissible strain of the monkeypox virus, is an emergency, not only for Africa, but for the entire globe. Mpox, originating in Africa, was neglected there, and later caused a global outbreak in 2022. It is time to act decisively to prevent history from repeating itself.”
Two vaccines for mpox are recommended by WHO immunisation experts.
The virus was first discovered in humans in 1970. It is transmitted to humans by infected animals but can also be passed from human to human through close physical contact.
It is the second PHEIC in succession on mpox — albeit one focused on a different, and more deadly, strain of the virus.
In May 2022, mpox infections surged worldwide, mostly affecting gay and bisexual men, due to the clade 2b subclade.
The WHO declared a public health emergency which lasted from July 2022 to May 2023. That outbreak has now largely subsided.

Concern over way deadly virus is spreading
Several outbreaks of different strains of mpox have occurred, the WHO said, with different modes of transmission and different levels of risk.
The clade 1b variant, which has been surging in the DRC since September 2023, causes more severe disease than clade 2b, with a higher fatality rate — around 5 per cent in adults and 10 per cent in children, compared to 3 per cent for clade 2b.
While the WHO said clade 1b appeared to at first be spreading mainly through sexual networks, worryingly, experts say the new strain is increasingly spreading through schools and workplaces via everyday touch.
“It is undoubtedly the most dangerous strain of mpox yet,” Professor Trudie Lang, the director of Global Health Network at Oxford University, previously told The Sun.
Jean Claude Udahemuka, from the University of Rwanda, who has been studying the outbreak, said there was evidence of transmission in schools and from mums or carers to children.
The disease appears to be causing miscarriages among pregnant women, as well as “horrendous whole body rashes” and other lingering symptoms. Previously, it caused lesions more limited to the genital area.
These significant differences from previous mpox strains were “incredibly worrying”, Prof Lang said.
“There is definitely the opportunity for this to get on a plane,” she added. “We need to be really vigilant now and try to move to contain it.”
A PHEIC has only been declared seven times previously since 2009 — over H1N1 swine flu, poliovirus, Ebola, Zika virus, Ebola again, Covid-19 and mpox.
Marion Koopmans, director of the Pandemic and Disaster Management Centre at Erasmus University Rotterdam, said a PHEIC declaration raises the alert globally.
“[But] the same priorities remain — investing in diagnostic capacity, public health response, treatment support and vaccination,” she said, warning that this would be a challenge as the DRC and its neighbours are lacking resources.
The International Federation of Red Cross and Red Crescent Societies said it was scaling up preparedness measures across Africa, notably in the heavily affected eastern DRC.
With its broad network, the IFRC said it was prepared to “play a crucial role in containing the spread of the disease, even in the hard-to-reach areas where the need is the greatest”.
— with AFP and The Sun
Originally published as Australia urged to take action in response to new mpox emergency





