Hopes new devices could vastly improve lives of sickest Australian diabetics
Artificial pancreases will be used in some of the sickest Australian diabetics amid hopes the devices could vastly improve their lives.
Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Artificial pancreases will be used in some of the sickest Australian diabetics amid hopes the devices could vastly improve their lives and pave the way for a wider national rollout.
While the insulin-pumping devices have been successfully trialled among relatively healthy Type 1 diabetics in recent years, it was thought artificial pancreases would struggle to overcome the complex complications faced by those with much more severe diabetes.
However, a world-first study led by St Vincent’s Hospital Melbourne will evaluate whether the rapidly evolving technology can improve the health of diabetics with advanced kidney disease – including those who must endure long sessions of dialysis every few days to stave off life-threatening complications.
With no functioning pancreas, severe Type 1 and some Type 2 diabetics must currently check their blood sugar levels four or more times a day and give themselves insulin injections to stabilise their glucose levels.

If the patients can instead be stabilised automatically by an implanted artificial pancreas St Vincent’s Hospital senior endocrinologist and lead researcher Professor David O’Neal said they would not only have a much greater quality of life, but save a fortune for health systems struggling to cope with increasing levels of chronic disease.
“It’s not the same as the healthy pancreas, but it’s closer to a healthy pancreas than injections and the fingerpicks,” Prof O’Neal said.
“Often these patients are older, they may have some degree of cognitive impairment, they may have complications, cardiac disease...they are frail people with some of the poorest quality of life.
“We feel that the burden of controlling their sugar level is very significant and something needs to be done to improve the quality of life – that’s why, for the first time, we want to try to use this very exciting and advanced technology.”
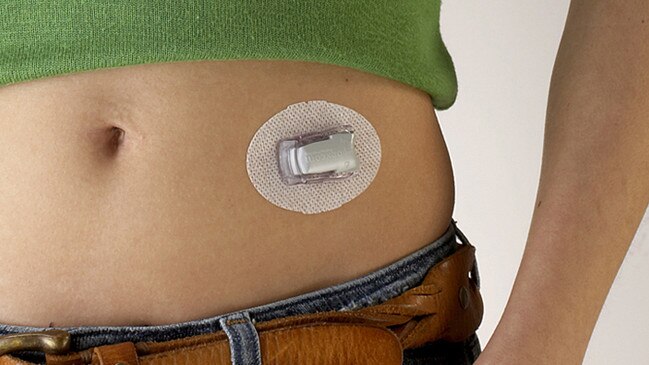
Known as a closed loop system, an artificial pancreas consists of a glucose sensor placed under a person’s skin that measures their blood levels every five minutes, before wirelessly transmitting the readings to a pump which adjusts the amount of rapid acting insulin it releases in accordance with the levels.
Some of the devices are now available commercially for a cost of $7,500-$8,5000 for patients with non-complex disease.

But over the coming weeks 40 Type 1 and potentially some Type 2 diabetics with advanced kidney disease in Victoria, South Australian and the ACT fitted with artificial pancreases and monitored for eight weeks.
If the closed loop devices can keep the patient’s glucose levels within a healthy range to slow the progression of life-threatening complications such as of hypoglycaemia, Prof O’Neal said it may provide the evidence required to push for government funding to provide artificial pancreases to those in the greatest need.
“If we show that there’s a significant improvement in sugar levels and quality of life and maybe even reduce the number of hospitalisations of people living with diabetes, this information may be used to leverage the government to say ‘we need to support these people by supporting provision of pumps’.
“Most importantly, the patient needs to feel better...that something life is worth living and they feel better in themselves. It’s not just all about sugar levels, it’s also about whether we are actually improving these vulnerable groups’ quality of life.”
The pilot is one of the first projects undertaken through the University of Melbourne’s new Australian Centre for Accelerating Diabetes Innovations, and was recently awarded the $150,000 Diabetes Australia Millennium Award to support the work.
Diabetes Australia chief executive Justine Cain said the world-first research provides renewed hope for the more than 270,000 Australians living with diabetes and kidney disease.
“The hope is that the artificial pancreas system Professor O’Neal and his team are researching will help people better manage their blood glucose levels while undergoing treatment for kidney disease and that this improves their overall health and quality of life,” Ms Cain said.
“Diabetes technology is one of the most exciting areas of diabetes research and we hope this project will help expand the ways it can support people.”


