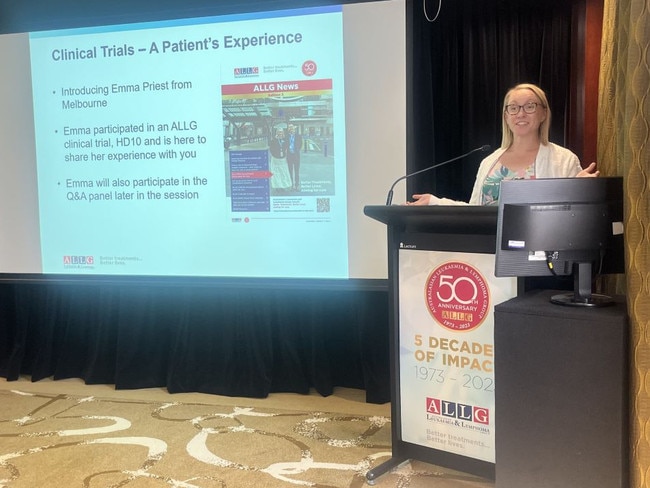
Melbourne nurse Emma Priest’s battle to beat cancer in a clinical trial
A Melbourne nurse received devastating news when what she believed was a simple infection was diagnosed as cancer. Instead of backing down, she faced the fight head-on.

West
Don't miss out on the headlines from West. Followed categories will be added to My News.
A Melbourne nurse received devastating news when what she believed was a simple infection was diagnosed as cancer.
St Vincent’s Hospital’s nurse Emma Priest started developing a low-grade fever and waking up in the middle of the night from night sweats, which she thought was odd because she was a healthy 38-year-old woman.
“It’s not that you feel hot or cold, you just wake up and you’re wet,” she said.
Ms Priest also had a persistent cough that only occurred when she was lying down in bed at night.
Curious to know what was wrong, she visited her doctor to hunt down whatever infection she thought she had.
Instead, after extensive testing, a chest scan revealed Ms Priest had enlarged lymph nodes, and she was asked to come to the emergency ward on the expected list.

“I went into quite the spin, as I used to work in an emergency, so I know what it means to be put on the expected list — something’s wrong,” she said.
“Cancer never popped into my head. I thought maybe I’ve just got some weird bug in my chest that I need special antibiotics.”
At the emergency ward, Ms Priest was told she had advanced Hodgkin’s lymphoma, an aggressive blood cancer.
“It was like being punched in the face to hear that because I didn’t feel unwell,” she said.
Ms Priest was told an 11cm tumour had wrapped itself around her aorta and oesophagus.
“I saw the mass of lymph nodes (in the scan), and it was pushing on my airway, causing the cough,” she said.

Ms Priest was given two weeks to do fertility preservation before she started chemotherapy.
Her doctor also told her she could participate in international clinical trial HD10 which was said to offer superior survival results, minimal side effects, no known impact on fertility, and a 50 per cent chance of less severe side effects.
Ms Priest said getting on the trial was a “no-brainer” and she started a four-cycle therapy, with each lasting three weeks.

After getting two cycles of very aggressive chemo, with Ms Priest only experiencing nausea, her doctor told her she was “in complete metabolic remission”, meaning the scans could not show cancer.
“I am immensely grateful for the trial and to have been able to work with clinicians who came up with ideas of how diseases should be treated,” she said.
“From day one, my treating team told me that we’ll get you through this, and it will be like a speed bump in your life.
“I can tell you that it didn’t feel like a speed bump then, but now yes, it was definitely a speed bump, and they got me through it.”
It’s been five years since Ms Priest finished the clinical trial, and she has now been declared “no longer in remission, meaning you are actually cured of the disease”.
“It’s like it never happened,” she said.
Prince of Wales Hospital haemotologist and veteran leader of blood cancer clinical trials Professor Mark Hertzberg AM said the superior outcomes of the clinical trial would change how Hodgkin lymphoma was treated around the world.
“Analysis of this study confirmed that, at four years, 94.3 per cent of BrECADD-treated patients remain free of disease recurrence,” he said.
“For patients who are PET-negative after two cycles (where no demonstrable disease can be seen), this rises to 96.8 per cent of patients who remain free of progression.”
Ms Priest said patients unsure about clinical trials should “take your time and read the information that’s been given”.
“Ask all your questions regarding the information you’ve been given,” she said.
“If the trial’s a good fit for you and it feels right — by all means, go for it. Because it might be the best decision you make.”




