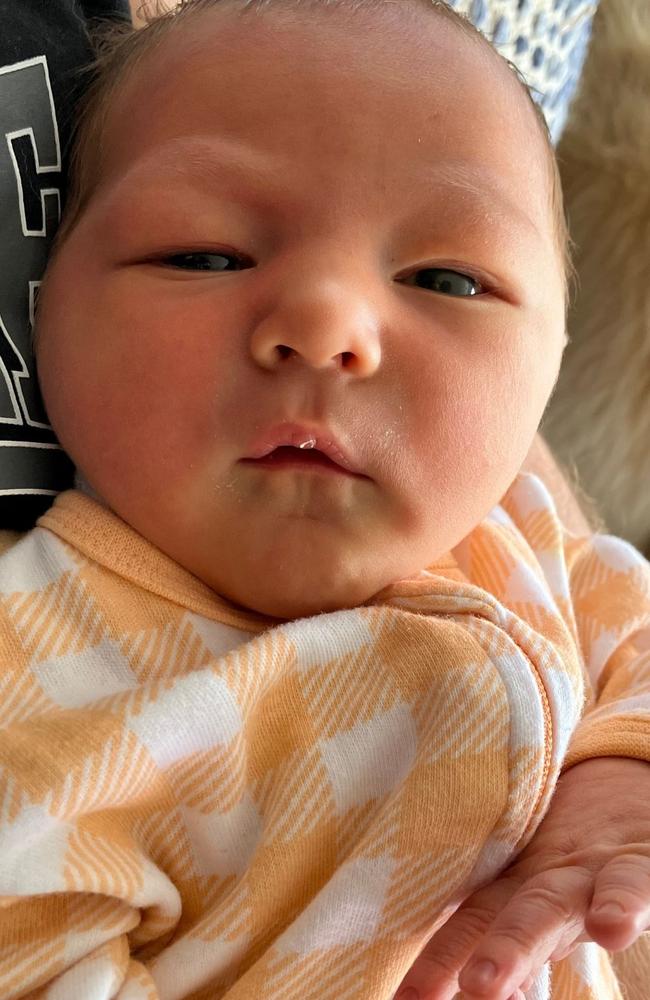
Pregnancy diary: Giving birth to my beautiful boy Beau
In the last instalment of Imogen’s pregnancy diary she details her birth, which had one scary moment, and meeting her gorgeous little boy, Beau.

Pregnancy
Don't miss out on the headlines from Pregnancy. Followed categories will be added to My News.
This is the last instalment of Imogen’s pregnancy diary.
See the previous chapters, released every Sunday, below.
Part one: Why I was dumbstruck when I found out I was pregnant
Part two: The first doctor’s appointment, blood tests and dating scan
Part three: Photo reveals why pregnancy announcement didn’t go to plan
Part four: I had these dreams about my baby’s gender
Part five: My family’s devastating loss while I was pregnant
Part six: Testing the wives’ tales about babies to see if they have any truth to them
Part seven: Coming to terms with the realities of giving birth
Part eight: How we chose the name for our son
Part nine: My frantic moment with ‘baby brain’
Part ten: I had pre-eclampsia and had to be induced
I was woken on Saturday January 11 at 5.45am.
I showered, had breakfast and was taken to the room where we would eventually meet our baby.
By 7am, I’d had the Foley balloon removed, a cannula placed, the CTG belts put on, my waters broken and the hormone drip started.
I recall the nurse was unsure if she’d managed to break my waters as there wasn’t a big gush of fluid.
However, when I got up to go to the toilet, the pinky-coloured water came rushing out of me, so yes, she had.
By 9am, Michael and Mum had arrived at the hospital, Mum with a coffee for me in hand.
So far, so good.
The birth playlist was on, the fairy lights were twinkling and I was feeling good.
I had to stop drinking the coffee though because it was starting to make me feel sick to my stomach.
I’d told the midwives my plan for pain – that I wanted to use lower levels of pain management like a TENS machine and the gas before considering an epidural (I really wanted to avoid morphine altogether) – earlier that morning, so now we were just waiting for the contractions to intensify.

Through the morning I’d been having period-like cramps and by about 10.30am I said to Michael and Mum that ‘I think we’d better get the TENS machine on’.
In the back of my mind I was also thinking that we’d better text Jordyn, the student midwife who had been following me through my pregnancy, about when to join us at the hospital.
Taking what I’d learned from the birthing classes, I was standing and leaning over the bed to get gravity on my side.
By now, the contractions were pretty intense, but still somewhat manageable with the TENS machine. The TENS has a boost feature which I pressed during the height of the contraction to send strong pulses to the pads on my back to distract and disrupt the pain signals to my brain.
I said, ‘If this is what it’s going to be like, then maybe I will need an epidural’.
Knowing my preferences, the midwife said, ‘how about you try the gas first and see how you go with that?’
‘OK,’ I said. It’s true that you lose all niceties when you’re in labour.
The gas helped immensely. You have to breathe into the mouthpiece normally and it gives you a short-lived high which ends once you breathe oxygen again.
I changed positions to kneeling and pressing back onto my heels.
‘How does that position feel, Imogen?’ the midwife asked. ‘Good,’ I said.
At some point, my pants had also come off but I was still in my T-shirt, not so much because I wanted to cover up but because taking it off would’ve been too much effort.
In fact, everything aside from giving birth was too much effort. I had my eyes closed because my brain didn’t have capacity to process what I was seeing. I didn’t care that my privates were out for all to see, the thought didn’t even have the audacity to cross my mind.
I was short and could only blurt out words like ‘water’, ‘text Jordyn’, ‘turn music up’ and my longest sentence, ‘this water bottle sucks’.
Sorry water bottle.
It is my ride or die water bottle that comes everywhere with me but in labour I needed one with a straw so I didn’t have to tip my head back to drink – because that was too much effort – and this one doesn’t have that. A plastic straw was eventually found.
‘Bubs isn’t liking this one so much, could we get you leaning over a birth ball?’ the midwife said of my kneeling position. ‘OK,’ I said.
Time loses all meaning in the birth suite, so at some point I managed to get onto the toilet – I think it was after the kneeling – and then waddle my way back to standing and leaning over the bed.

And this is where I remained.
I was breathing the gas like it was going out of fashion. I was in the room, but I wasn’t. I could hear everyone around me, I could hear the music, I could feel Michael holding my hand, I could hear Mum giving me words of encouragement but I was on a different planet.
I wasn’t getting much of a break between contractions so my mouth remained on the gas mouthpiece for basically the entirety of the labour. I was only able to come off for at most about five seconds between contractions, as the pain briefly subsided.
I think this is because my body reacted strongly to the synthetic hormones.
Through the birth, I recall hearing the midwives saying they had reduced the amount they were giving me, eventually stopping the drugs all together as my body had taken over and was contracting on its own.
Because of this reaction, the labour was progressing quickly.
I kept hearing the midwives saying I was doing really well and that it was going by fast. One of the midwives said she thought I’d have the baby by the end of her shift.
Hearing that, I thought to myself, ‘OK, if this is going to only be another hour or so, I can do that’. I was feeling good – as good as you can be in labour – and empowered. It was encouraging to hear that I was handling it well and it was going quickly.
Additionally, when I’d earlier said about needing an epidural the midwife had told me that I’d need to stay very still in order to have the epidural placed and I was in no position to sit still.
So, powering on with the gas it was.
I had Michael’s hand, Mum’s words of encouragement – she could have a career as a doula! – and Jordyn – the text was sent! – on water duty.
Then the urge to push came.

The best way I can describe this feeling is that it’s similar to when you’re vomiting hard and your body keeps contracting, even though there’s nothing coming up.
You don’t have any control over those impulses, you just have to ride them out.
It’s a similar feeling except the motion is pushing down rather than up.
As I was standing, each time the urge to push came my knees would bend forward and my hips would dip down.
I groaned into the gas mouthpiece, biting down on the plastic.
The midwives checked my dilation and I was 8cm, so they encouraged me to try and breathe through the urges so as to not push down on my cervix until it was fully dilated to 10cm.
The next time they checked me, the baby’s head was crowning, so I was given the all clear to go with my body and push when I needed to.
So when the urges came, I was pushing hard. Riding the wave that my body gave me, sometimes I got one big push and other times it was a big one quickly followed by a smaller quicker one.
‘C’mon Imogen we need a really big push here,’ the midwives were saying.
I thought, ‘I am pushing! I can’t push any harder than this!’
I was trying to catch my breath after each push to push harder and they were still wanting more.
‘All right Imogen, big push, come on!’
The midwives’ words were becoming more urgent.
I kept pushing but I felt like I wasn’t getting anywhere, I couldn’t feel him moving down.
Then all of a sudden, I felt two hands inside me and then the baby was pulled out of me.
I saw a big splash of blood go on the floor, heard a little baby squeak and then a midwife said to me, ‘we’re going to have to cut the cord Imogen.’
Michael and I had hoped that we’d be able to do delayed cord clamping – which allows additional nutrients to pass to the baby after birth – and that he’d be the one to cut the cord.
Everything was happening behind me but I could hear that something was up.
The midwife said, ‘he’s just a little shell shocked from birth, we’re just giving him some help to breathe’.
I didn’t hear the code blue get called but the room was suddenly full of people.
Michael said all he could see of our baby was a little blue arm on the resuscitation table.
As all this was going on, I was being helped to take my T-shirt off and get onto the bed. So oblivious was I to everything that was happening, my main concern was not slipping in my blood on the floor.
I got into the bed and my baby, now breathing, was placed onto my chest.
‘What’s his name?’ the midwives asked.
‘Beau,’ I said. ‘His name is Beau’.
I was completely overwhelmed. I cried from joy, from exhaustion, from relief, that our boy, Beau Bailey Worrall, was finally here.
He was born at 3.46pm on Saturday January 11 after 4 hours and 55 minutes in labour.
However, our time together, skin-to-skin, was short lived because he was having a bit of trouble breathing.
He was grunting and working hard to breathe, so the doctor said it’d be best to take him up to the special care nursery for monitoring to make sure he could breathe properly.
He also had a bruise on his left elbow from where he’d gotten stuck on the way out, so they wanted to examine that too.
So the doctor, Michael and Beau left Mum and I in the room.
Now it was time to deliver the placenta.
I’d opted for active third-stage management, which is where you’re given synthetic oxytocin – the same that’s used to induce labour – to deliver the placenta as soon as possible after the birth.
The midwives tugged on the umbilical cord to encourage it to come out but it wouldn’t budge.
They got me to go to the toilet in the hopes that gravity would get it out. No luck.
They put a catheter in to drain my bladder because sometimes the placenta gets stuck behind a full bladder. Still nothing.
There were talks of having to go to theatre to get the placenta out.
The doctor said the last option was to see if she could feel it to manually remove it.
So up in the stirrups I went again.
She said that my cervix had begun closing as the placenta was on its way out and it had gotten stuck as it was being delivered – deja vu.
But she managed to slowly pull it out. Theatre avoided … or so I thought.
She then said it was time to check for any tears.
Lo and behold, I’d managed to give myself a third-degree tear.
The scale of tears has four as the worst kind, so a third-degree tear was pretty serious.
So down to theatre I went to have that repaired. If I’d had an epidural, I could’ve been stitched up in the room.

With the spinal tap placed, I laid back and felt my lower half go completely numb. That is a very bizarre feeling, seeing someone touch your leg and having no sensation of it at all.
I closed my eyes and the anaesthetist asked if I’d like to listen to any particular type of music. I said I didn’t mind so she put on some jazz.
I remember lying there thinking ‘oh my God, I’m lying on my back, I haven’t done this in months.’ It was so nice.
Once I was all stitched up, Michael joined me in recovery. Mum had gone to the NICU to be with Beau.
Michael said Beau was doing well and we would visit him on the way down to the ward so I could have my first breastfeed.
Once we were finished feeding in the NICU I was taken to the ward and Beau joined me at about midnight.
We’ve been together ever since.
Originally published as Pregnancy diary: Giving birth to my beautiful boy Beau


