Three years ago, Hannah Smith was a happy and healthy 46-year old – she was working four days a week as a psychologist, a career she loved; she and her partner Michael had purchased a house in West Hobart; she was travelling interstate regularly to visit her adult children and her grandchildren; and the roller derby enthusiast had also just been selected to compete nationally. Life was good.
But then Smith contracted Covid-19, in April 2022 – and her life took a dramatic turn for the worse, signalling the start of an almost three-year battle she describes as a “nightmare” which, at its worst, left her housebound, bed-bound and led her to question whether life was worth living.

“We went to Melbourne for our friends’ wedding,’’ Smith recalls.
“We got home and Michael tested positive for Covid. I felt fine, but I tested, and I was positive as well. A couple of days later, I had a headache and a slightly stuffy nose, that was it.’’
Or so she thought.
“I was tired the next week so I decided to work from home by telehealth. I was just exhausted,’’ Smith recalls.
She’d recently been through two stressful life events – a friend’s son died and a family member had a health crisis – so at first, Smith assumed her exhaustion was due to the emotional toll of those events.
But the exhaustion didn’t ease, despite her taking a couple of weeks off work to rest, and a barrage of strange symptoms appeared.
Smith had migraines. She had gastrointestinal problems. She had insomnia, and struggled to sleep for more than 40 minutes at a time. Her body temperature felt out of whack, as did her emotions. Usually “cheerful and outgoing”, she suddenly felt overwhelmed and couldn’t stop crying. Her periods stopped. Her arm would tingle, and then go numb.
They were all “weird” symptoms Smith hadn’t experienced before.

Her GP ran “all sorts of tests” – checking for things like glandular fever and vitamin deficiencies – but “everything came back normal”.
Meanwhile Smith had become dizzy with vertigo, and her “heart felt weird”.
“The brain fog was awful,’’ she says.
“Light, sound – everything was overstimulating, I couldn’t watch television, I couldn’t read a book. I’d get up and go to work, and then I’d come home and go to bed, that was all I could do. I stopped showering and started having baths.’’
After three months, a GP recognised Smith likely had long Covid, and referred her to the state government’s Post Covid-19 Navigation Service, where a telehealth nurse called every six weeks to check on her progress. She says she was so exhausted that even talking on the phone was an enormous struggle.
The only other help she qualified for was a cleaner once a fortnight from Anglicare.
“It has been a nightmare,’’ Smith says.
“My GP, when I was first sick, told me it was really important to keep working. I did half days until the end of 2022, by which time I couldn’t move, think, or speak. Eventually I had to resign from my employed position after a year’s leave without pay. We have been financially devastated, and are struggling with mortgage payments.’’
She had income protection insurance but was unable to make a claim due to the delay in getting a long Covid diagnosis, and has spent $50,000 worth of savings. Her partner works long hours to bring in additional income, and for the past two years they have moved into a shed on her father’s property over summer so they can rent out their home on Airbnb to help make ends meet.

Smith would like to see greater financial support for long Covid sufferers. She’d also like to see long Covid become a notifiable disease so there would be a way to collate data on the number of people affected.
“There needs to be better medical care. And there needs to be better community understanding,” she says.
Smith has lost friends and rarely goes out.
“When I ‘overdo’ things – which might just be cooking a meal and doing the washing on the same day – I have migraines and often can’t move from fatigue for a few days,’’ she says.
“My mental health has suffered enormously, which is not a problem I’ve ever had before. But it really has felt that life wasn’t worth living at times. I just thought I’d get better, because I always did get better from everything I’d had in the past.
“Life (before Covid) had been great. I was earning more than I’d ever earned, I was travelling overseas and interstate, I’d bought a very expensive house. But I got to the point where I couldn’t leave the house and I thought my partner should leave me because I was a burden.’’
Fortunately things began to improve when Smith discovered Clinic 19, a telehealth clinic in Victoria, specialising in long Covid.

Finally, she was talking to a doctor who was knowledgeable about long Covid, who was sympathetic to her struggles, who was quickly able to identify that Smith had common Covid-related conditions like POTS (postural orthostatic tachycardia syndrome) and symptoms including PEM (post exertion malaise) and – most importantly – offered hope for the future. “She knew of things that would help,’’ Smith says.
“It was a pivotal moment; it was amazing, I felt hopeful that I might recover, or even just recover some quality of life.’’
Smith started taking low-dose naltrexone, a medication commonly used in the treatment of long Covid as well as conditions like fibromyalgia, Crohn’s disease and multiple sclerosis.
“Within three days I had an hour where my head cleared and I felt like myself,’’ she says.
“It was a sign of hope. I now have a period most days where I feel normal.’’
She is again working as a psychologist – two days in person and one day at home. She used to see seven or eight clients a day but now sees between two and five clients, allowing 30 minutes between each appointment to rest.
“I am pretty useless the rest of the time,’’ Smith says.
“I don’t go out in the evening, and spend much of my time laying down. I don’t know if I will ever be a healthy person again. But I already feel I can live a life that is worth living. I can go for walk on the beach; I can see my family.’’

Smith is just one of many previously healthy people in Tasmania – and around the globe – who identify as having long Covid, an often baffling array of symptoms that continue months, or even years, after the initial signs of Covid infection.
And she is one of three Tasmanian sufferers sharing their stories exclusively with TasWeekend to coincide with International Long Covid Awareness Day, on Saturday March 15.
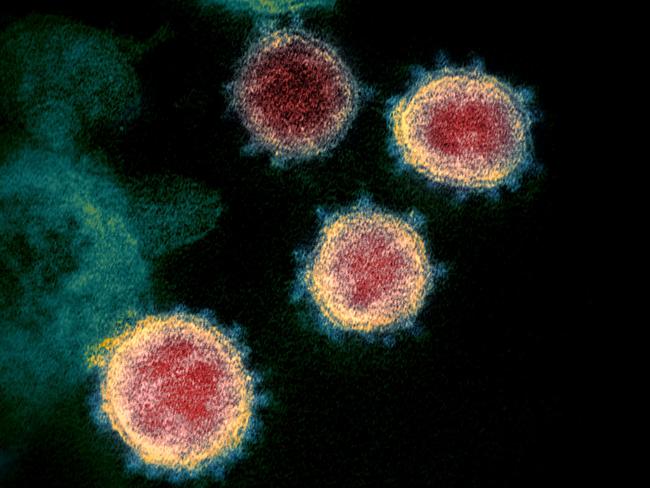
The World Health Organisation defines post Covid-19 condition – commonly known as long Covid – as “a condition that occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually three months from the onset of Covid-19 with symptoms that last for at least two months and cannot be explained by an alternative diagnosis.’’
It says common symptoms include fatigue, shortness of breath, cognitive dysfunction, changes in taste or smell, chest pain, difficulty sleeping, anxiety or depressions and headaches – although more than 200 different symptoms have been reported – which “vary between individuals”, may “fluctuate or relapse over time” and “generally have an impact on everyday functioning”.

Although exact numbers of those living with the condition are uncertain, studies suggest about 10 to 20 per cent of people affected by Covid may go on to develop long Covid symptoms, and estimates suggest about 5 per cent of the global population have long Covid.
Meanwhile a study of 11,000 Australians who tested positive to Covid, by researchers at Australian National University, revealed almost one in five experienced ongoing symptoms three months after their initial diagnosis.
Studies suggest long Covid is more common in women. Research has found a strong overlap between myalgic encephalomyelitis/chronic fatigue syndrome and long Covid, along with fibromyalgia, a chronic pain disorder.
Some studies suggest long Covid can trigger diabetes, coeliac disease and other auto-immune conditions, while others link it to ongoing cognitive and psychiatric problems.
Researchers have put forward a number of theories about the root cause of the illness, whether that’s microclots, cytokine storms, histamine intolerance, gut microbiomes, lingering spike protein in the body, or dysautonomia (a dysfunction of the nerves that regulate non-voluntary body functions such as heart rate, blood pressure and sweating).

Some suggest a component of the virus may live in the gut of some long Covid patients, causing persistent inflammation, vagus nerve dysfunction and neurological symptoms, while playing havoc with the body’s nervous systems.
But regardless of the exact cause, long Covid has huge repercussions on public health and productivity.
A joint study by The University of Melbourne, the Australian National University and UNSW Sydney estimated Australian workers living with long Covid cost the economy about $9.6bn in 2022, as a result of 100 million hours in lost labour.
Meanwhile globally, researchers estimate long Covid has affected 400 million people worldwide – a number they say is conservative – at an economic cost of about $1 trillion annually, which is equivalent to 1 per cent of the global economy.
TASMANIAN GP Dr Toby Gardner says long Covid is a “hidden epidemic” and more funding and medical research is needed to better understand the condition and provide better support for patients, as well as for the doctors treating those patients.
The Tasmanian chairman of the Royal Australian College of General Practitioners, who owns two large group practices in Launceston and is the director of their affiliated urgent care clinic, says he personally sees at least one patient a week with symptoms of long Covid – are he’s just one doctor in a larger practice of 30-plus doctors, who are also seeing patients with long Covid.
When you consider there are about 600 GPs in Tasmania – and about 40,000 nationally – who are likely seeing similar numbers of patients with the condition, that’s a significant number of Tasmanians – and Australians – struggling with long Covid.
“Absolutely, we’re seeing patients with symptoms that would be consistent with long Covid,’’ Dr Gardner says.
“We know it’s impacting people across the nation and it needs to be taken seriously.’’
Dr Gardner says the tricky thing about long Covid is that there is no single diagnostic test.
So doctors rely on a process of elimination, running various tests and ruling out a raft of other conditions, before making a long Covid diagnosis.
Some patients he sees have respiratory or cardiac issues. Others face chronic fatigue or cognitive impairment, struggling with significant brain fog that sometimes requires them to take extended periods away from work or school.

He’s treated doctors with symptoms consistent with long Covid who can no longer work due to cognitive impairment and has referred patients to Clinic 19, where a range of treatments are used including low-dose naltrexone, co-enzyme Q10, nicotine patches and H1 and H2 antihistamines.
“It can be an invisible illness for a GP,’’ Dr Gardner says.
“We’re still learning. There’s lots about Covid itself, as well as long Covid, that we still don’t know.
Which is why the RACGP is pushing for funding to update guidelines for doctors to inform treatment as new evidence comes to hand.
He’d also like to see more funding for medical research and eventually hopes there will be some sort of diagnostic test for long Covid, with tailored treatments.
“It’s certainly a moving feast of information,’’ he says. “We’re constantly trying to keep up and we’re certainly treating it seriously. We don’t know the prevalence of this. But I imagine it’s a hidden epidemic out there, the more we can talk about it, the better educated the general public and our medical professionals are going to be.’’
He urges anyone who has unexplained medical symptoms following a bout of Covid to consult a doctor.
“It’s a real thing and if you’re suffering symptoms that can’t be explained by conventional tests and you can tie it to when you had Covid and are wondering ‘is this long Covid?’ then you should discuss it with your GP,’’ Dr Gardner says.
The Tasmanian government launched a Post Covid-19 Navigation Service in September 2022 as part of a $400,000 commitment to support Tasmanians with long Covid.
The telehealth service – run by qualified health professionals who can help patients self-manage ongoing symptoms and provide referrals to allied health services like physiotherapy or social services – is available to Tasmanians 16 years and older by referral from a GP, and operates as an extension of the government’s virtual Care@home program, which supports Tasmanians with Covid and other respiratory illnesses.
A government spokesperson says since 2022, the Post Covid-19 Navigation Service team has supported 211 patients, with 192 discharged and 19 currently enrolled.
The service expanded in February 2024 to offer a new breathing retraining program for patients who would benefit from this therapeutic intervention.
“Tasmanians who continue to experience Covid-19 symptoms more than 12 weeks after they started are encouraged to visit their GP or usual healthcare provider to confirm their diagnosis and discuss the Post Covid-19 Navigation Service,’’ the spokesperson says.
JILL SAUNDERS says the most difficult thing about having long Covid is that it’s largely an “invisible illness” and many people – including some doctors – still fail to recognise it as a valid condition.
She feels she is living a “shadow life” – and she also feels strongly that the government should do more to recognise long Covid, invest more money into research and treatment options and better support those who are suffering.

Just because she’s not in a wheelchair, or doesn’t have an obvious physical disability, doesn’t mean Saunders, and others like her, aren’t struggling.
“You’re completely ignored because people can’t see it – you haven’t got a bone sticking out of your leg,’’ she says.
“People with long Covid are treated like freaks and are left to deal with a medical system that doesn’t believe they are ill, because of the constellation of symptoms that go with this condition. I find it difficult to understand that the government won’t recognise long Covid as an illness. It leaves us in this nether world, with no cure, no treatment, nothing. It’s just horrendous. People are dying. But worse than dying, is the living coffin that you’re in – you’re living this shadow life. It’s just a catastrophe.’’
The 68-year-old, who founded organic skincare business Beauty and the Bees 32 years ago, has had to take a step back from her business and rely on staff to take on some of her duties as she no longer has the energy or cognitive ability to work at the same level she once did.
She has endured two years with dysgeusia, an altered sense of taste, which has significantly reduced her quality of life.

She has lost 17kg, is unable to eat a healthy, balanced diet as there are limited foods she can tolerate (avocado on plain bread is a current diet staple), and food tastes “absolutely disgusting” and makes her nauseous.
Long Covid has also been costly – in addition to the many supplements and medications she has tried, Saunders spent $5000 on an interstate medical procedure in June last year, which was not covered by Medicare or private health insurance, in the hope it would restore her sense of taste.
And while that stellate ganglion block, administered by a pain specialist at a private hospital in Melbourne, did significantly reduce symptoms like anxiety, brain fog and gastrointestinal upsets, Saunders says her taste issues remain.
“It’s an example of how desperate people are to find something that is going to help them,’’ she says of having the costly procedure.
Saunders had Covid in December 2022.
“I felt unwell, about three or four days before Christmas,’’ she recalls.
“I got a test and it confirmed I had Covid. I live alone, so I just survived the best I could – it was the most miserable Christmas ever. I lost my sense of taste – everything tasted absolutely disgusting.’’
She seemingly recovered from the initial infection, but unfortunately, it was only the beginning.
She struggled to find a GP who could help her, and initially turned to online long Covid groups to find out as much as she could about the condition from others who were also struggling (the Australian Long Covid Community Facebook group has more than 5000 members, while the Long Covid Support Group has more than 67,000 members).
“Few medical practitioners have got any idea at all about this affliction, so we are left to reference each other on these Covid groups – we are left to learn from each other,’’ she says.
Saunders, who has autism and ADHD, says she has “quite pronounced cognitive damage” since having Covid and works largely from home in Lindisfarne.
“Working within my business has been increasingly difficult,’’ she says.
“I had to put staff into place and bring in consultants at huge expense to help me run the business. Because at the end of the day I cannot make decisions the way I was, I have to have everything simplified. I can’t look at spreadsheets any more, I can’t make sense of spreadsheets, everything has to be dumbed down. It’s very difficult. And there is no end in sight and that is a problem. It’s not as though I’ve broken my leg and I’ll be off work for a period of time and then I’ll be back. There’s no end in sight – no help, no discussion, no information.’’
She now sees an integrative medicine doctor and says low-dose naltrexone has helped bring some of her energy and focus back.
She says while altered taste may seem minor compared to what some others with long Covid are experiencing, the impacts are wide-reaching.
“I used to travel all over the world,’’ she says.
“But now, what’s the point? There’s no point travelling, there’s no point taking holidays, there’s nothing to look forward to; life is very black and white and it’s a massive struggle.
“Every day I put off eating as long as I possibly can, so I don’t have to endure it. And I’m on the same diet – there’s no more eating out, friendships have folded, people don’t want to hear about it. It’s very isolating, it’s extremely difficult to deal with and it’s very depressing.’’
Saunders says she was “as fit as a mallee bull” before getting Covid and is sharing her story in the hope it will help others feel less alone while also prompting greater support for long Covid sufferers.
“I want to raise awareness that this is a real thing, affecting 400 million people worldwide. It’s not something just a few people have,’’ she says.

“There are thousands upon thousands of people suffering in silence with no help whatsoever.
“The most important thing is, the government needs to recognise this and do something about it. Billions of dollars need to be thrown at this. Set up clinics, do some exploratory research, and most importantly recognise that people’s lives are being destroyed. There are people out there who can’t work, who are not surviving financially, who get no recognition from the government.
“Other medical conditions are recognised and you get dispensation for illness, but there’s no recognition of long Covid and that, for most people, is the most wounding thing. You can’t get any understanding from anybody that this is not made up.
“I want recognition of this as a genuine disorder that is causing the country a huge financial loss. And also recognition of the distress and the destruction of people’s lives … they just live these grey lives that were previously lived in full Pantone colour.’’
Another frightening thing about long Covid is the impact it can have on young people.
EVELYN BAEHR was only 13 when she contracted Covid in April 2022, and the now 16-year-old has spent almost three years dealing with crushing bouts of brain fog and chronic fatigue, as well as a fast heart rate due to an autonomic nervous system disorder.

She wears ear plugs as she is oversensitive to sound and light.
Confident and outgoing, Evelyn has had to give up much loved activities like archery and theatre group. She rarely sees her friends. She has had to reduce the number of hours she studies each day. She often struggles to do simple math equations that she previously found easy. She wears a heart monitor. She spends long periods in her room resting. And she feels that she is missing out on spending quality time with her younger siblings.
She feels like she is being robbed of her teenage years.
“It definitely feels like I’m being set back so much and missing out on so many experiences,’’ says Evelyn, who is homeschooled and lives on the outskirts of Huonville.
“In the beginning I didn’t want to let go of those things (like archery and drama), but I know that what’s more important is to focus on getting better. I’ve had a strong immune system my whole life, I hardly ever got sick. Never in a million years would I have expected to get something like this.’’
Evelyn was visiting family in the US when she contracted Covid at a party.
“The whole family got sick, but for me, it was a bit different,’’ she recalls.
“I was just feeling super unwell, it was weeks long, and I thought ‘this is weird, I guess it’s just taking my body a bit longer to get over this’.’’
After any sort of exertion, Evelyn was exhausted and would need to lie down and rest, something that was extremely unusual for the active teen.
It took many months, and many blood tests from numerous doctors, before a doctor suggested she may have long Covid.
A referral to Clinic 19 followed, and after a long wait to secure an appointment, Evelyn says she finally felt heard and understood.
She was diagnosed with POTS which helped explain her racing heart rate. She was prescribed low-dose naltrexone, which helped her brain fog, and she also takes heart medication.
She says one of the problems with being a child with long Covid, is that some of the medications that are being used successfully to help adults haven’t yet been tested on children so can’t safely be prescribed.
But she says the low-dose naltrexone has made a huge difference to her quality of life.
She says if she went to a friend’s house, or to a doctor’s appointment, she used to crash for a week or two. Now, thanks to the medication, if she does too much, she typically only crashes for a day or two at most.
It’s still far from ideal for a 16-year-old who longs to be a regular teenager and has dreams of becoming a professional voice actor.
But at least there are steady signs of improvement.
“It’s hard to watch,’’ admits Evelyn’s dad Peirce Baehr of her struggles.
For her 16th birthday on January 1, Evelyn’s parents threw her a large birthday party at the local hall, to make up for the two previous birthdays she had missed celebrating due to
ill-health.
Evelyn finds online support groups helpful and has had Zoom catch-ups with other long Covid kids across Australia in the past. She is also committed to raising awareness about the condition and her voice features as part of an international awareness campaign created in the UK which aims to highlight the impact long Covid has had on children.

Figures show 110,000 children in the UK are living with long Covid, while in the US that figure is estimated to be 5.8 million.
Evelyn’s grandmother, Margaret Sonnemann, also has long Covid, as do some members of their church community.
“Often if you don’t have a member of your family or friends with long Covid it can be really hard, even if your family is super supportive,’’ Evelyn says.
“Because you can’t really understand it when you don’t have it.
“So many doctors don’t understand or don’t even believe that it’s a real thing. It’s really upsetting how many doctors don’t know, or don’t make an effort to know a little bit to at least refer you to other people.
“For both the medical community and just people in general – there needs to be more awareness about it.’’ •
If this story has raised any concerns for you, contact Lifeline on 13 11 14, Beyond Blue on
1300 224 63 or contact your GP.
For details about the state government’s
Post Covid-19 Navigation Service visit – coronavirus.tas.gov.au/COVID19-recovery

Add your comment to this story
To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout
Swansea’s Indian gem makes welcome return for summer
Head to Swansea. Order everything. Thank me later – as you won’t want to miss out on this terrific little East Coast pop-up, writes Alix Davis
Ultimate guide to what’s on in Tassie this summer
Summer is coming! Make the most of the warmer weather with our go-to summer events guide – it’s packed with must-do Tassie activities to enliven your social calendar and kickstart 2026 in style