‘Unsustainable:’ Shock number of Victorians waiting for vital surgery revealed, as ambo crisis worsens
Victorians in need of surgery say they’ve been “robbed” of years of their life as waiting lists continue to blow out amid the state’s health crisis.

Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Ambulance Victoria has failed to meet more than a third of code one calls within the benchmark response time, while people were forced to wait longer in the emergency department for urgent treatment.
New quarterly data, released on Saturday, has revealed the state’s long elective surgery waitlist dipped slightly from 88,920 patients between January and March, to 87,275 in the most recent quarter which covered the April and June period.
It’s an increase of more than 21,000 people when compared with the same time last year. In April and June 2021, the waitlist was sitting at 66,230.
Just 73 per cent of elective surgeries were being performed within the recommended wait times over the past three months, dropping from an 81 per cent average between January and March.
The long-awaited quarterly healthcare performance data shows Victoria’s paramedics are busier than ever, with 97,928 code 1 call outs.
Only 64 per cent of code 1 cases were responded to within the 15 minute benchmark. The target is 85 per cent of calls.

It’s the busiest quarter on record, with a 16 per cent increase – or 13,487 more “lights and sirens” cases – compared to the same time last year and the third consecutive quarter where code 1 demand records have been broken.
Ambulance Victoria interim chief executive Felicity Topp said there are “no signs of demand slowing down through winter”.
“Our paramedics are working extremely hard to manage the increasing demand while prioritising care to the sickest Victorians,” Ms Topp said.
The number of people presenting to the emergency department also hit record highs, increasing by 5.1 per cent – to 486,701 people in total – between April and June.
Wait times in the emergency department also increased, with code 1 patients now forced to wait 20 minutes on average.
In the previous quarter, and at the same time last year, the median wait time was 18 minutes.
Code 1 incidents require urgent paramedic and hospital care, while code 2 incidents are acute and time sensitive but do not require a lights and sirens response.

Australian Medical Association Victoria president Roderick McRae said hospitals are overwhelmed and he suspects the real figures are much higher.
“I’d suggest that the ED presentations are an underestimate, because many people approach the hospital and see queues and go away, or they sit in the queue for a while, and they’re not attended to . . . and they leave.
“We’re getting more and more reports of people spending in the order of 10 hours, give or take a few hours, until they’re seen.
“The emergency departments are really moving to a mash-like disaster management system . . . . they’re not able to look after people to the capacity they know they’re trained to, and that they want to.”
Dr McRae said the elective surgery waiting list was also likely higher in real life, pointing out there are likely people who meet the clinical requirements but are yet to see, or get into, a medical specialist who can refer them.
“It’s problematic to get in to see a specialist to then add the next step to be put on the waiting list,” he said.
“(A quarterly decrease) doesn’t completely gel with the reports that we’re getting.”
He said the increase in emergency department presentations was “no surprise” and the government had ignored experts’ warnings.
“We were coming into winter,” he said.
“The strong advice was it was the wrong time to let up on any community management relating to Covid.
“That advice was ignored and of course the stresses on the healthcare system have only increased exactly as predicted.”
The increase in emergency department presentations comes after the Royal Children’s
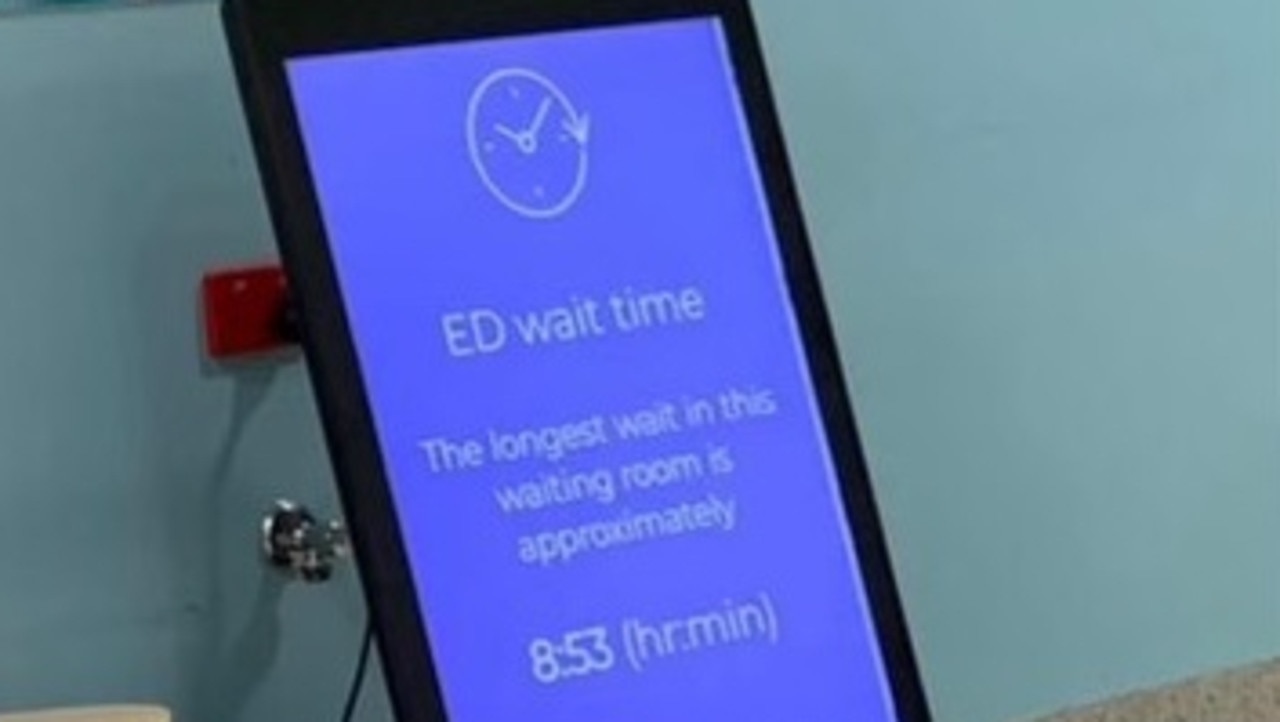
Hospital’s emergency department had wait times of up to almost nine hours on Monday, with one doctor saying it was the busiest he had seen in his 30-year career.
The Andrews government has long spruiked the unprecedented demand on the healthcare system has been caused by Covid – and staff being furloughed – but experts warn years of underfunding has been the root cause and is now exposing the cracks.
There are currently less than 700 Victorians in hospital with Covid, the lowest point since July. In January this year, 1200 people were hospitalised with the virus.
Of the state’s 100,000 odd healthcare workforce across the public sector, between 1400 and 2000 staff – or about 2 per cent – are absent each day due to Covid.
And of Ambulance Victoria’s 5500 paramedics, the rolling weekly average of paramedics furloughed is between 164 and 246.
Victorian Healthcare Association head of policy and advocacy, Juan Paolo Legaspi, said extreme demand on the system appears to be the “new norm” in Victoria.
Mr Legaspi said it was time for governments to do more to address the workforce shortage in our public health system.
This shortage, which existed before the pandemic, has worsened with furloughing due to Covid- 19, and increasing rates of burnout, he said.
“We can’t just keep asking healthcare workers to ‘keep on going’ when we know this won’t be the last wave of Covid,” he said.
“This data shows we are in an unprecedented era of intense demand.
“Our health workforce is under high pressure all the time. It’s unsustainable. Unless we bring in a lot more workers to reduce this burden quickly, we’re at risk of losing staff faster than we can recruit or train them.”

Ahead of the November Victorian election, the VHA - which is the peak body for public hospitals - has called on the Andrews government to create a workforce strategy and recruitment campaign to “urgently attract more health workers locally and from overseas”.
Victorian Ambulance Union general secretary Danny Hill said paramedics were “just getting smashed”.
“I’m not at all surprised that the response times have deteriorated badly,” he said.
“It takes a huge toll (on our members). Let’s just remember they’re absolute heroes.
“Ambulance is often used as a political football, they’re delivering some of the best care that we see anywhere in the world.”
He warned the increased pressure on emergency departments - up by 24,742 compared to the last quarter - make it more difficult for paramedics to hand their patients over to hospital staff.
This forces them to continue caring for patients in car parks as they wait for a bed to free up - a process called ramping, he said.
“Ambulance ramping occurs every day,” he said.
“We’re going to have this problem as long as emergency departments are being used as a one stop shop.

“So long as everyone’s coming in through that door, we’re going to have ambulance ramping, and it’s happening right across Australia.”
Mr Hill said he was concerned response times may continue to worsen, but said he was hopeful recent investments such as expanding referral pathways to redirect non-urgent patients away from emergency departments and paramedics, will help.
“This is not about putting more paramedics or more ambulance crews,” he said.
“It’s about targeting funding areas aimed at reducing demand in our health system.”
Health Minister Mary-Anne Thomas said the latest release of quarterly performance data confirmed Victoria’s health system is still under “unprecedented pressure”.
But she added that “it’s improving slowly”, and the elective surgery waitlist had “stabilised”.
“We’re in the midst of a record-breaking period of demand on our health system, but this latest data shows that we are weathering the storm and building a system that will be stronger than ever moving forward,” she said.
“We’ve never pretended there’s a quick fix.”

‘They robbed me of seven years of my life’
An elderly man who has been on a surgery waiting list for nearly a decade said delays have “robbed” him seven years of his life.
76-year-old John Rawlinson first developed acute lower back pain caused by a herniated vertebra in 2015.
Mr Rawlinson was placed on a waiting list at a public hospital and was introduced to “pain management” in the meantime.
“Seven years spent waiting and the injuries have become chronic, leaving me crippled to the extent I can barely hobble to the bathroom from the adjoining bedroom,” Mr Rawlinson said.
In January this year Mr Rawlinson was promised corrective surgery within 90 days.
“They are already 50 days over scheduled time limit, and still stalling with any excuse possible,” he said.
The Sunshine West resident said the health system was “savage”.
“This is what can be expected when someone is on public funded elective surgery, to be cultivated into a full blown cripple,” he said.
“It was a treatable injury ignored for seven years.
“I was kept as a permanent patient for the purpose of government assisted funding and treated with painkillers – knowing the true nature of the injury but financially ignoring their responsibility.
“They robbed me seven years of my life.”

‘I struggle everyday’
Elyas Rezaee said he has “given up hope” on receiving surgery to remove inflamed polyps from his nose after being left on the waiting list for more than two years.
The 23-year-old Hampton Park resident is unable to sleep at night or exercise due to a fear he could stop breathing at any moment.
“My breathing is heavily restricted, my right nostril is completely blocked by polyps,” Mr Rezaee said.
“I struggle everyday with normal activities such as playing sports or running.”
Mr Rezaee said he is forced to use a nasal spray in the meantime while waiting for surgery.
“The spray I use shrinks the vessels in my nostrils, but after a couple of hours the vessels come back doubled in size,” he said.
“I have to have the spray on me 24/7.
“I wake up six to seven times at night when the spray starts to wear off.
“I’ve also got tooth decay now because I have to breathe through my mouth at night.”
He said his condition has “gotten a lot worse” while he has been on the waiting list for over two years.
“I keep going back to my GP to tell them how bad it was getting and they moved me from a category three to a category two.”
“I’ve ultimately given up hope on receiving surgery.”
More Coverage
Originally published as ‘Unsustainable:’ Shock number of Victorians waiting for vital surgery revealed, as ambo crisis worsens








