We need to talk about the m-factor
Hobart GP Dr Hannah Chapman says there’s no need for women going through perimenopause and menopause to suffer in silence these days, writes Eleanor De Jong

Tasmania
Don't miss out on the headlines from Tasmania. Followed categories will be added to My News.
When Alexandra from Hobart first walked into her GP’s office with symptoms that had left her feeling a shadow of herself, she was hoping for answers.
Instead, she left feeling unheard. It would take years before she’d understand that her headaches, muscle aches, fatigue, and brain fog were symptoms of perimenopause, the hormonal transition that billions of women around the world endure in silence.

“It’s such a gradual, insidious thing,” recalls Alexandra, describing the onset of symptoms that chipped away at her wellbeing. “For a long time, I didn’t even realise they were symptoms. It just seemed like I was having more and more ‘bad days.’ Despite how brilliant my GP is, I felt she didn’t have the necessary knowledge to help me navigate or manage what was happening to me.”
Alexandra’s experience is far from uncommon. Menopause, the natural transition marking the end of a woman’s reproductive years, often leaves women feeling not only physically unwell but also emotionally and mentally adrift. As the ovaries cease their monthly cycle, women’s experience of the transition varies widely. The rare few breeze through with hardly a symptom, while others find themselves grappling with life-altering changes that affect work, relationships, and their mental health.
Even the rich and famous aren’t immune.
“I felt like I was losing my mind, and I was definitely losing what it felt like to be ‘myself.’”Australian actor Naomi Watts told Hello magazine.
“I truly believe that if menopause hadn’t been such an off-limits topic when I first started experiencing symptoms, I would’ve had an easier transition. But at the time, I felt like I was the only one going through it, and that isolation just made things worse.”
According to the World Health Organization, postmenopausal women are one of the fastest-growing demographics globally, thanks to increased life expectancy. Yet, the medical understanding and societal support for this group are lagging sorely behind.

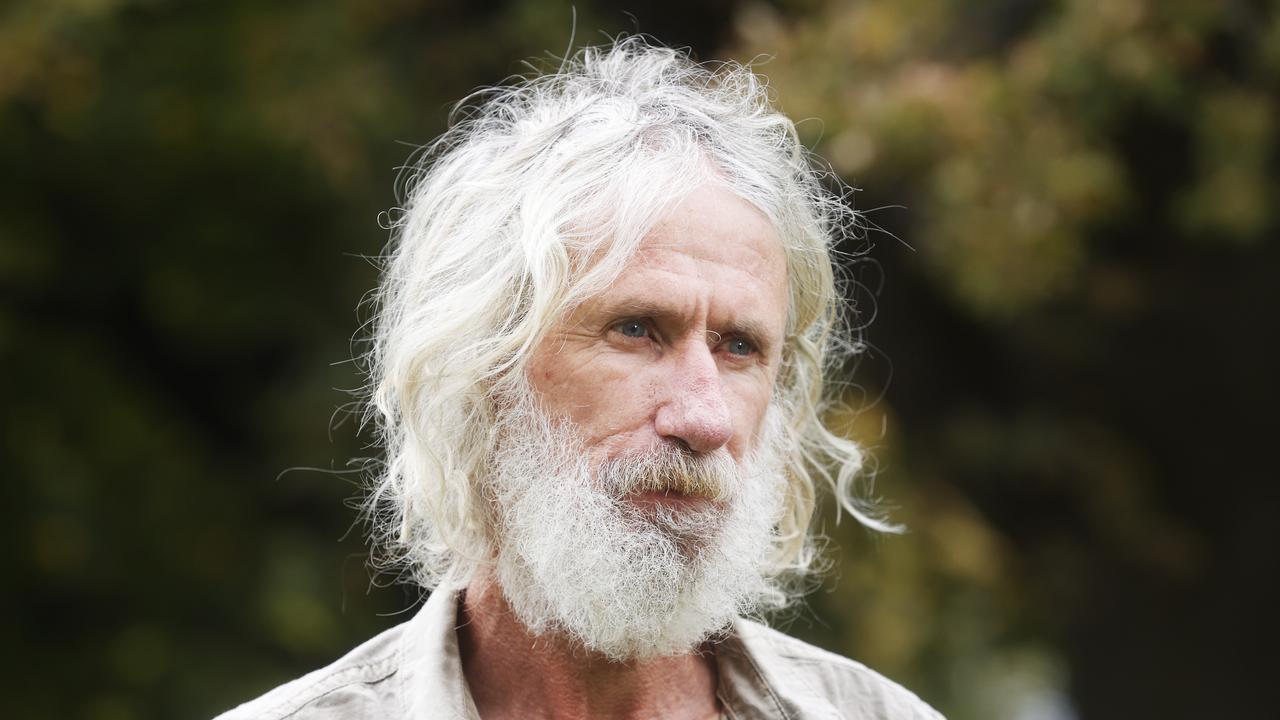
A DOCTOR’S PERSONAL CONNECTION
Dr Hannah Chapman, a GP based in Hobart, spent nearly two decades helping women with their reproductive health before experiencing a wake-up call of her own. In her early 40s she entered perimenopause, and experienced treatment-resistant depression that led her to re-evaluate the way she and other clinicians treated menopause.
According to the latest data, there is a 16-fold increase in depression in women aged between 42 and 52. Astoundingly, the peak of female suicide is between the ages of 45-49, according to the ABS.
“During my training years, I was not aware of that kind of bias toward men’s health,” Chapman reflects. “I was just in a system and learning it. I look back now and think, isn’t it wild that I wasn’t taught about menopause during my medical degree?”
Chapman’s own experience trying to find relief for the symptoms of perimenopause have now culminated in the establishment of Tasmania’s first-ever dedicated perimenopause clinic. Now aged 47, Chapman says she is the “healthiest, happiest and most productive I have ever been”, a state of mid-life she wants all her patients to experience.

The clinic, tucked away on Hobart’s Macquarie St, is a peaceful sanctuary-type space designed with comfort in mind. The lush plants, cosy lounges, and a curated selection of books help create a soft, non-clinical vibe.
“I wanted women to feel welcomed in a way that clinical healthcare spaces rarely allow,” she explains. “I have tried to create an intentionally non-fearful space for women who are already not feeling their best. Here, I want them to feel safe, comfortable, and soothed from the outset. And just to know that they’re going to be on a positive journey.”
MENOPAUSE, REFRAMED
In her clinic, Chapman has reframed menopause from a dreaded and embarrassing phase of life defined by hot flushes and night sweats, to an age where women can thrive and flourish, with the right help.
“There are several points in a woman’s life when her hormones will fluctuate quite wildly,” she says. “Puberty, pregnancy, and perimenopause. The first two are sort of celebrated – people are supportive. But with perimenopause, we’ve been remarkably silent until now. Women are expected to just deal with it quietly, to soldier on.”
Alexandra was among the clinic’s early patients, seeking answers after years of pain and frustration.
Today, thanks to hormone replacement therapy (HRT) as well as estrogen and testosterone, her life has transformed.
“My symptoms have almost disappeared,” she says, noting that testosterone – not widely available in many countries – has been a game-changer. “I’ve got quality of life back; it’s made a huge improvement for me.”
Since opening, Chapman’s clinic has been so overwhelmed with demand that she’s booked out months in advance. However, she plans to expand the clinic’s offerings in the New Year.

RECLAIMING JOY, STRENGTH, AND SELF
Some of the women who visit Chapman have internalised their struggles so deeply that they hesitate to seek help.
She believes this reluctance is not “innate” but stems from a history of dismissal of women’s health problems, from painful periods to undiagnosed endometriosis and more.
“What I see every day in my practice is women who are just not feeling themselves,” she says. “Sometimes they’ve lost their ability to feel joy. They’re tired, they’re aching, they’re sore. Their mood is low, they might be experiencing anxiety for the first time in their entire life, and finding it quite the blindside. And yet, they’re so good at internalising all of it, at explaining it away and adapting around it, that they often never seek help.”
Chapman says even when women do ask for help from the medical establishment, their concerns can be dismissed or overlooked. This observation is backed up by a growing body of research, including a landmark study of menopausal women in the UK which found eight in 10 respondents said their workplace had no basic support in place and 41 per cent said menopause symptoms were treated as a joke by colleagues.
“Women are told menopausal symptoms are just part of getting older or that they should just tough it out. But it doesn’t have to be that way. Helping women feel like themselves again – that’s always my goal.” Chapman says.
The same study also found it took “many GP appointments” to be diagnosed with menopause or perimenopause, an experience that is familiar to Alexandra.
But since seeing Chapman, her recovery has been profound.
“I feel like I have my life back,” Alexandra says, adding that she is enjoying work again, and her friends and family have told her: “You’re so much happier now. And I really am”
And for Chapman, there’s no better reward than helping her patients feel better.
“I am passionate that women really can thrive during midlife,” she says.
“It doesn’t just have to be a time of, as Germaine Greer would say, ‘mourning’.
“It can be a time of growth, of renewal, of rediscovering who you are. And that’s what I want to help every woman achieve.” •
Dr Hannah Chapman’s clinic is located at
174 Macquarie St, Hobart. For inquiries about appointments and/or more information
phone 6204 9596.

EVERYTHING YOU NEED TO KNOW ABOUT MENOPAUSE
Dr Sarah White, the chief executive of Jean Hailes for Women’s Health, and GP Dr Judith Hammond explain everything about menopause – from hot flushes to life after periods
WHAT IS MENOPAUSE?
Menopause is when a woman’s menstrual periods stop because her ovaries are no longer producing eggs.
In Australia, the average age of menopause is about 51 years of age and it’s 12 months after your final menstrual period. You no longer have menstrual periods and you can’t get pregnant.

HOW IS IT DIFFERENT TO PERIMENOPAUSE?
The lead-up to menopause is called perimenopause and this is when the levels of hormones start to go up and down and then tail off into what is called postmenopause.
Perimenopause typically starts when a woman is in her 40s, but can begin as early as the mid-30s or as late as the early 50s. It usually lasts about four years.
For some women, perimenopause can be over quickly, for others it can last up to 10 years.
The key sign that you’ve entered perimenopause are changes in your menstrual cycle.
If you use contraception that stops your periods, you might not notice any changes and it’s important to remember that for some women, they don’t go through perimenopause.
They enter the postmenopausal period abruptly as a result of surgery or medical treatment.
WHAT’S THE GOOD NEWS?
For many women it is a real relief to no longer have periods. For those who’ve had migraines and acne associated with periods, it’s often fantastic not to have to put up with those anymore.
We no longer have to worry about contraception and for some women who have never really found a form of contraception they’ve felt happy with, they can have sexual activity without any worries.
We are older and wiser and we’re often reaching a stage in life where we’re starting to feel much more comfortable with ourselves.
Menopause can be stressful, but it can also be a positive time.

WHAT ARE THE SYMPTOMS?
There’s a lot of open discussion these days about the impact of menopausal symptoms, which is a really positive step forward.
The most common symptoms include hot flushes and night sweats, mood swings and increased irritability, trouble sleeping, vaginal dryness and changes in libido or sex drive.
The menopausal transition affects every woman differently and you may experience some, all or none of the symptoms.
About one in four women won’t have any symptoms, about one in four will have severe menopausal symptoms and the remaining one in two will have symptoms that range from mildly annoying to difficult to manage.
They typically start in perimenopause, the lead-up to the final menstrual period. However, some women are unlucky enough to get symptoms continuing well into the post-menopausal period. Women who have surgical menopause don’t go through perimenopause at all – they have a sudden onset of menopausal symptoms.
There’s no doubt the menopause transition can be a challenging time, so if you are experiencing symptoms that are interfering with the quality of your life, see your doctor.

GET HEALTHY
This is also a great time to reassess your lifestyle factors to help you both to manage symptoms and to stay fit and healthy after menopause.
It’s about regular exercise, a balanced diet, reducing alcohol and stopping smoking, along with reducing stress levels and maintaining healthy social connections.
Prioritising sleep is also important.
When looking for information, find credible sources that are not trying to sell you anything. Make sure it is evidence-based and aligned with professional menopause society information.
BE PREPARED, NOT SCARED
We talk about being prepared, not scared of menopause because for many women it’s an empowering life transition not having to worry about contraception and periods, particularly for women who have heavy, irregular or painful periods.
Many women tell us they feel a new sense of personal growth and wisdom as they enter the post-menopausal stage of life.
For more information visit: jeanhailes.org.au/health-a-z/menopause
More Coverage
Originally published as We need to talk about the m-factor