Obese patients requiring surgery need more access to weight loss drugs
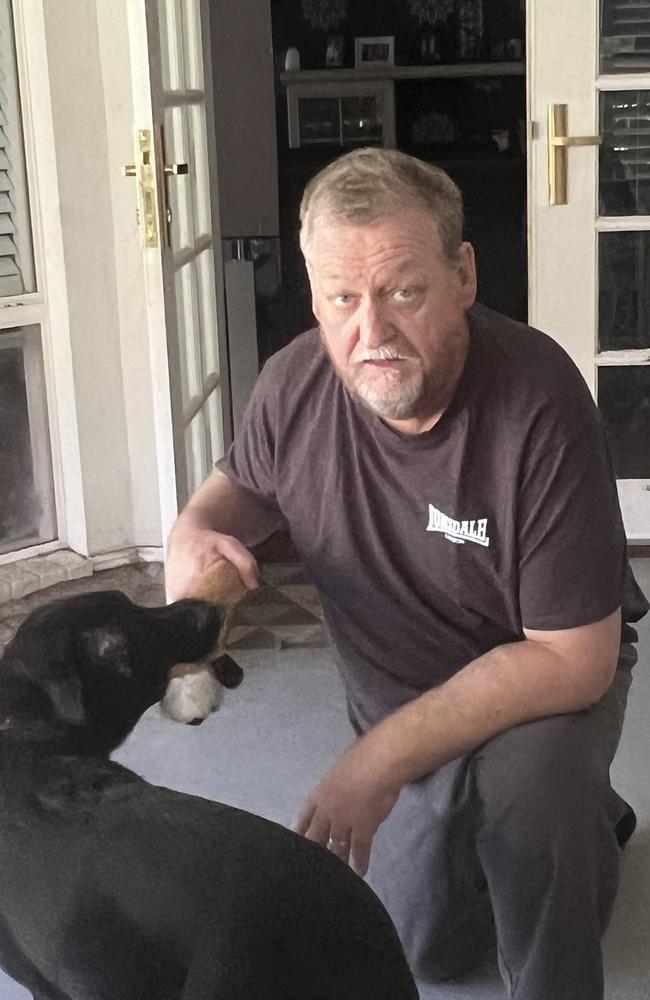
David Fardon needed a kidney transplant, but his high BMI increased his risk of surgery. This is how he lost 30kg.

Weight Loss
Don't miss out on the headlines from Weight Loss. Followed categories will be added to My News.
For three years David Fardon missed out on family weddings, holidays and a social life because he had to do dialysis.
Suffering from kidney failure, the 55-year-old from Packenham in Melbourne’s south east was waiting for a kidney transplant.
The trouble was he was obese, weighing in at 150kg, increasing his risk if he was to undergo surgery.
He first tried diets to lose some of the weight, but only managed 10kg before he plateaued.
Then he started taking Mounjaro in May last year and it helped him lose 30kg.
“I reached my goal weight and I got put on the list. I had to wait six to eight weeks (for a kidney to become available), which was very quick,” he said.
Mr Fardon said prior to surgery he was part of a small group of people doing dialysis for three years.
“During that time four of the people doing the program with me passed away, it was really daunting,” he said.
“I missed out on family weddings and I never went away on holidays because I would be on dialysis.
“I’m now going on my first holiday in a few weeks and I have a better quality of life. I really have a new lease on life.

“Unfortunately, someone had to pass away for me to continue living but they have given me a bigger gift than I could ever have hoped for.”
Specialists say that overweight people who have cancer or need a transplant are using weight loss medication before the life-saving surgery to reduce risk of complications.
They are now calling for drugs like Ozempic and Mounjaro to be included on the PBS for use in pre-surgery and pre-transplant patients who are overweight, warning that some people could be at risk of missing out on getting help because they can’t afford it.
Juno Healthcare chief executive and gastroenterologist Associate Professor Suong Lee said the service had helped 200 obese patients by putting them on weight loss drugs before their operations.
“The type of patients we were seeing were those where obesity had caused the condition and they needed the surgery to cure the condition but it was too risky to do the surgery,” Assoc Prof Suong said.
“If your BMI is over 35 then you have a higher risk of a longer operation time, infection and staying in hospital longer due to other risks associated with surgery.”
Assoc Prof Lee said there could be some initial side effects from taking the drugs like nausea and reflux.

She urged the federal government to make the drugs – which can cost between $150 and $500 per month - more affordable for people needing life-saving surgery.
“We are ethically concerned that because of these drugs, the only people that can afford them in order to lose weight for surgery are the ones who have the money to do so.
“What we would like to see is that these drugs are on the PBS for short-term use cases for high risk patients before lifesaving surgery.”
Gastroenterological Society of Australia (GESA) board member and immediate past endoscopy faculty chair Dr Matthew Remedios said these types of GLP-1 drugs represented an “exciting advancement” in managing diseases linked to being overweight.
“The literature is evolving rapidly in support of this class of medications in obesity, type 2 diabetes, cardiac, renal and liver disease,” Dr Remedios said.
“(We) support educating both medical practitioners and patients on the role of these medications in disease managements and the equitable access to these medications at affordable pricing when appropriately indicated.”
University of Melbourne’s Dr Zina Valaydon, who is a gastroenterologist and hepatologist at Western Health, said using weight loss drugs in pre-operative settings was an “emerging area”.
“We know that the anaesthetic risk for them is significantly lower including those experiencing less cardiovascular risks and respiratory problems,” Dr Valaydon said.
She said some degree of judgment should be exercised when using weight loss drugs in pre-operative circumstances.
“The main issue remains as to when do we stop these drugs prior to going under anaesthetic and we have been fairly conservative in the past.
“To my knowledge there hasn’t been any studies into adverse events of people who were actively on those drugs and underwent a major operation.”
A Therapeutic Goods Administration (TGA) spokesman said patients should adhere to the advice of their GP and specialist prior to taking any medication leading up to surgery.
“Tirzepatide (marketed as Mounjaro) and semaglutide (marketed as Ozempic and Wegovy) are glucagon-like peptide-1 (GLP-1) medicines,” he said.
“As with all medicines, GLP-1 medicines can cause side effects (also known as adverse events).
“Common, but usually not severe, side effects of these medicines include nausea, vomiting and diarrhoea. More serious, but less common, side effects can include allergic reactions, severe stomach pain, and other issues that might require medical attention.”
It’s understood the TGA is reviewing the guidelines to do with weight loss drugs and changes will be finalised later this year.
More Coverage
Originally published as Obese patients requiring surgery need more access to weight loss drugs









