Quest for immunity is the fight of our life
Why do we shake off some diseases easily but are defenceless in the face of others?
There is a simple question the experts who study viruses do not always relish being asked. The question is this: what is it that makes one disease give you lasting immunity, while in another it is fleeting?
“That is complicated,” says Shane Crotty, from the La Jolla Institute for Immunology in California.
“That’s really difficult,” agrees Deenan Pillay, professor of virology at University College London. “You would have to speak to a geeky immunologist about that.”
Dan Davis is professor of immunology at Manchester University, author of The Beautiful Cure, a book about the immune system, and a fully accredited geeky immunologist. “This is a crucial frontier that is shortly going to be of paramount importance,” he begins rather more promisingly. And his answer? “The truth is, it’s a really important gap in our knowledge. It’s a little bit mysterious.”
There is no shame in this — scientists happily admit that sometimes they operate at the edge of knowledge. But it is, nevertheless, a shame. Because as Davis suggests, this question is really rather important.
On it hangs trillions of dollars and tens of thousands, perhaps hundreds of thousands, perhaps even millions, of lives. If an antibody test shows you have had coronavirus, does that mean you are immune to coronavirus? And for how long?
How immunity happens
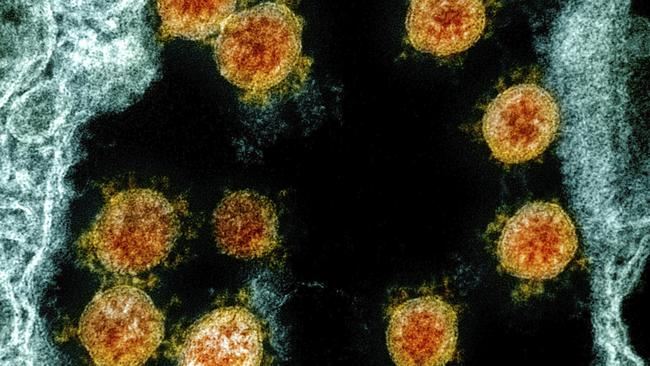
Late last year, almost certainly in China, a human experienced something that had previously happened to no human in the world. A submicroscopic mix of protein molecules entered his or her body, found a cell in the throat or nose and inserted some genetic material to hijack it. This material was a code, 30,000 letters long and those letters in that precise sequence had never been inside a human. They were the new coronavirus.
In response, this human did something commonplace that is also extraordinary. So long as he or she survived, this person, this Patient Zero, not only fought it off, but found a way to attack it uniquely now and probably also in the future. In the process he or she gained the antibodies that today are being tested for around the world.
Here is the standard description of how that happened.
In the body are cells called B-cells. On the surface of each cell are thousands of identical turrets of protein. Each turret is seeking its match — another protein, floating in the body, that will slot perfectly on to it, locking on.
On every individual cell, these turrets are identical. But each cell is different. And there are a lot of them. When a new B cell is made, its genes are shuffled to produce a new turret with a slightly different shape. This process can make 10 billion different flavours of turret. Enough, in fact, that there is pretty much nothing that can enter your body, whether virus or bacteria, to which there will not be a B-cell that can lock to it. Eventually, your body will find a match to one part of the coronavirus.
The immune system, in its complexity, is often called elegant. This first step, though, is not an elegant solution. It is deeply inelegant. It is what hackers would call a brute force attack, the equivalent of trying every password combination until you alight on the right one. But it works. When the B-cell finds its match it is activated and starts replicating.

Some of the copies it makes become factories, churning out soluble versions of those turrets — which we call antibodies — that lock on to the coronavirus. Antibodies can neutralise the virus directly, by stopping it being able to get inside a cell. They also flag the virus and infected cells for destruction by other immune cells. Some of these antibody-producing cells become “memory” cells, ready to mount a new defence if needed again.
And so it is that you become immune. How long for depends on how long your body decides to keep those cells and antibodies circulating. Sometimes it decides they are worth a long-term investment, sometimes not.
When describing the immune system, it is hard not to talk of armies and soldiers and battles. But the mundane truth is, it is about atoms and structures that mindlessly lock and interlock.
Why, in this wholly deterministic process, do we not know what happens next? The truth is, it is just too complex to understand that way.
“The immune system is incredibly complicated,” says Eleanor Riley, professor of immunology and infectious disease at Edinburgh University. “Because it’s so important to us, it cannot have a single point of failure. There are loads of ways the body can see a virus, think ‘I don’t like this virus’, and get rid of it.”
There are many parts of a coronavirus that a turret can lock on to, and there are also many methods — not covered in this simplified explanation — to do it. She likens it to a pinball falling through a machine. “There is no single path to the bottom. Put in a coronavirus, and like the pinball we know it will end up at the bottom, with immunity. But for every person it will do it differently.”
When the ball lands there may be the flashing lights that mark a high score — long-term immunity. Or it may get diverted into the gutter of temporary immunity, leaving you reaching for coins to put in the slot, and preparing to do it all over again.

Route to lasting immunity
Smallpox is the only disease that has ever been eradicated in humans. Towards the end of the 20th century, thanks to a vaccine, a virus that once killed a third of those infected, and infected two-thirds of the population, disappeared from the planet. The benefits in terms of human suffering are incalculable.
There is also a comparatively small benefit to virology. Unlike with any other virus, we can be sure that since the 1970s no one has been re-exposed to it. For Crotty, this was useful. He looked for antibodies in those who had been given the vaccine in the last wave. He found the antibodies were still there, as strong as ever.
“As far as we can tell, people have memory of smallpox for 40-plus years, and it didn’t really change between year five and year 40. Those cells are just circulating in people’s blood.”
And yet, he adds: “We definitely know of other cases where we’ll have an immune response, and it’s essentially undetectable after three years.”
Worryingly, some of the most ephemeral immune responses, lasting just months, come from coronaviruses. Not the coronavirus that has gained viral celebrity in the truest sense of the term but from those that cause a sniffle rather than a pandemic, part of the cocktail of viruses we call the common cold.
Yet look at another coronavirus still — the one that caused the deadly SARS outbreak of 2002 — and not only are antibodies still circulating in people, but they may even offer some protection against the new pandemic.
So which category is this latest coronavirus, the superstar coronavirus, going to fall into? The best clue comes not in what the viruses look like but in what they do. Do they leave you reaching for a tissue? Or for a ventilator?
“This immune memory may work like any other memory,” says Alessandro Sette, from the La Jolla Institute. “In life, if it’s a very traumatic event, you tend to remember it more.”
In this idea, Riley says, “the body needs to say, ‘Eh-up, there’s something here I need to pay attention to’. If a virus causes little damage, if it gets into your nose but goes no further, there may just be a trivial response.”
Here, there is both good news and bad news for the coronavirus. For those worst affected the disease is severe enough that the likelihood is we will have a proportionate immune response — that the healthcare workers incapacitated by it this winter will not have to endure it next winter. But there is another corollary. Just this week we learnt that up to 70 per cent of people barely get a symptom. Will they also have long-lived immunity? And does it matter if they don’t?
That depends, Riley says. “Was it mild because they are not at risk? Or was it because they did not get much virus to start with? If the former, there’s no need to worry.” If the disease does not affect them, then it does not matter if their immunity fades. “If the latter, if it’s just because they got a glancing blow, then next time they might not be lucky.”
What does this mean for vaccines?
If there is one question more important to the world right now than whether getting the virus gives you immunity, it’s whether getting a vaccine does. A vaccine is a medical trick. It is a benign deceit performed on your immune system. Most of us are familiar with the first part of its trickery — how the vaccine takes on the clothing of the virus, but in a deactivated form.
There is a second trick, a bit less well known and a bit more mysterious. This is the adjuvant. Early in vaccine development, scientists found, for reasons they could not explain, that the drugs just worked better if they were mixed with other chemicals. This makes a kind of sense. It is not enough that the body spots a foreign invader, it also has to believe it is dangerous — it has to think, in Riley’s words, “There’s something here I need to pay attention to.” This is what the adjuvant does.
The main bit of a vaccine is an imitation of the virus, and the adjuvant imitates danger. Different adjuvants work in different ways but overall, they all jump start an immune response. They are feints, mobilising the body against a phony army — so it is ready in force for the real one.
“Crucially, the adjuvant, and many other aspects of a vaccine, could all be tweaked to give a strong response, even if coronavirus itself doesn’t,” Davis says.
Andy Pollard is part of the team developing the Oxford vaccine. They have evidence from previous work that their approach will work — precisely because they can boost the response in this way.
“There is some cause for optimism there will be a lasting response,” he says.
But he won’t go further than that. “I can’t prove it until we have done the studies, and that needs months and years.”
Ultimately, for vaccine-induced immunity and infection induced immunity alike, there is only one sure test. Wait and see.
The Times







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout