Dying scientist Ralph Steinman rolled the dice
After centuries of cut, burn and poison, could a vaccine cure cancer? Pioneering immunologist Ralph Steinman bet his life’s work on it.
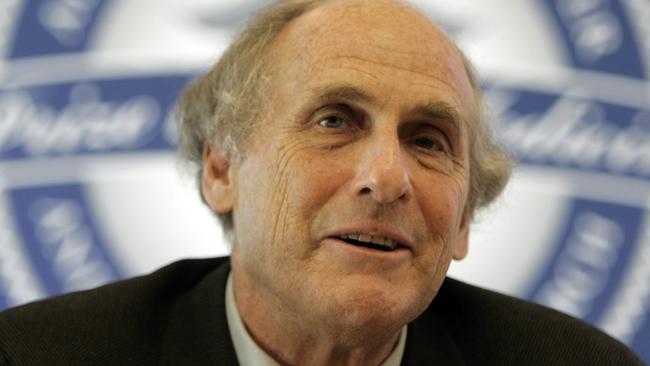
Ralph Steinman did not know how much time he had. He did know, though, that it would be enough for his last and greatest experiment. In the northern spring of 2007, Steinman was diagnosed with stage four pancreatic cancer. He told his family not to Google it – the prognosis was bleak. Very bleak. The doctors would perform surgery, but they warned him the cancer would return, metastasise and spread.
One way of looking at this was that Steinman, 64, had just been told he was going to die. The way Steinman, a pioneering immunologist, looked at it was ever so slightly different: that he had nothing to lose. It was the perfect opportunity to test his life’s work.
When the tennis-ball-sized tumour was removed, it was not binned but it was sliced and diced, parcelled, packaged and posted. Bits of it found their way to seven laboratories on two continents. From these laboratories – staffed by Steinman’s old students, old rivals and old conference friends – came back novel therapies, exploiting what are called dendritic cells, which Steinman had discovered earlier in his career.
Those therapies were the most experimental of treatments, an approach to cancer dreamt of for more than a century and which has had many false dawns. They are the class of therapy Ugur Sahin and Ozlem Tureci – inventors of the technology behind the Pfizer Covid jab – predict is sufficiently mature that by 2030 it would become a standard treatment. Into his veins, Steinman had injected cancer vaccines.
There are, researchers used to say, three pillars of cancer treatment: cut, burn, poison. First came cut. Hippocrates described removing tumours. “That which medicine does not heal,” he wrote, “the knife frequently heals.” And frequently it didn’t. For two millennia, that was all we had. Then in the early 20th century came burn. Early with radiation we learnt it could cause cancer, but by 1910 scientists were investigating ways radiotherapy could cure cancer.
Last came poison. During World War I doctors noticed that soldiers who had been attacked with mustard gas had very low white blood cell counts. This led to an idea: what if we could treat cancers of the immune system with the chemical? It formed the basis of the first chemotherapy, using chemicals to stop cancer cells dividing.
This is the conventional history of 20th-century cancer, but it needn’t have been so. In 1890 William Coley, a doctor newly graduated from Harvard Medical School, was assigned a 17-year-old patient called Bessie Dashiell. Dashiell had a malignant bone tumour. Surgeons removed her forearm, but it was not enough. The cancer metastasised, spreading throughout her body, and she died.
Coley considered her death preventable. He researched the case of a man whose neck tumour, seven years before, had disappeared when he contracted a bacterial infection. He then discovered 18th-century syphilis patients had lower cancer rates and became convinced that the body itself was killing the cancer – in a kinder, more natural way.
Cancer cells are not your cells, they are perversions of your cells. They have become, in a sense, foreign objects. In our body, we have a system to attack foreign objects: the immune system. Coley’s proposal was that somehow these patients’ infections had reactivated the immune system, allowing it also to attack the tumour. More than that, perhaps the body is always attacking – or trying to attack – cancer cells. Coley was ignored, but he was right.
Belatedly, immunology has become the fourth pillar of cancer treatment. We can target antibodies. We can genetically tweak cells to help them recognise cancer. And we can remove the brakes on the immune response that ordinarily allow cancer to spread unseen. To defeat smallpox or protect against measles, we had a cheap, simple and proven answer: a vaccine. Why couldn’t we do the same for cancer? Why couldn’t we train the body to target the bits of cells that are unique to the cancer someone has and then defeat it? Sounds simple, but it has proved extremely hard to implement.

Virus cells – say of measles, smallpox or rubella – are easy to spot. Cancer cells evade the immune system because they don’t look very different. Only a few of the proteins they express on their surface, which are the bits you would want to train a vaccine to attack, are different enough to form targets. But when you find those proteins, the immune response from the vaccine has to be really powerful, much more so than when responding to a virus.
At about the time Steinman was being injected with his experimental cancer vaccines, two Turkish immigrants in Germany were working on a different technology they thought could deal, at last, with the problem in a methodical way. Sahin and Tureci, husband and wife, had met while working at a cancer hospital. They were frustrated that the old paradigm – cut, burn, poison – was failing. Worse, it was brutal on the patients. They wanted to do more, and thought of vaccines. “(Researchers) have had this thought for 100 years,” Sahin told me earlier this year. “We stimulate the immune system, do something magic, and the tumour disappears.” The problem was “we had to solve the ‘something magic’ ”. The couple, whose company was called BioNTech, thought the magic was a molecule called mRNA.
There is an idea so important it is known as the “central dogma of molecular biology”. It is this: DNA makes RNA makes protein. These five words explain much of what happens in your body. In the centre of your cells is a string of DNA. This is a bit like the Ikea instruction manual but for making proteins. But the DNA is not, on its own, enough. An Ikea manual is no good without the person to read it and the flatpack they turn into a bookshelf. This is where messenger RNA, or mRNA, comes in. It is like the person reading the manual. It takes the instructions and brings them to the place where they can be acted on – where the proteins can be assembled.
Sahin and Tureci realised mRNA was a way of hijacking cells. Give them the mRNA we choose and the cells will make the proteins we want. And if the proteins we choose are those on the surface of cancer cells, we could train the immune system to target and destroy them.
There was an additional advantage to this approach. Because the RNA is just code, it is easy to change. Rather than looking for the vanishingly rare protein common to all cancers, you can find one specific to each patient and make a personalised cancer vaccine. It was a bold, simple idea. But there was the niggling thought. Simple ideas had a tendency to fall apart on meeting the complexity of the immune system.
Steinman had become famous because of an odd little cell. Spiky and starlike, it looked like a weird tentacled sea creature. He called it a dendritic cell (dendron is Greek for tree), after the branching pattern he saw under a microscope. When he first spotted it in the 1970s, many of his colleagues felt it was unimportant - yet another oddity in our unimaginably complex immune system. But he persisted to discover what these cells did. In doing so, he discovered they were the missing link in a longstanding puzzle.
When a virus, say, infects a body, it is fought off using T-cells and antibodies. But these are not enough. How do they learn what to attack? The answer was dendritic cells, which identify foreign proteins and present them as a target list. When Steinman learnt he had cancer, it was natural that the mechanism of these cells would be what his colleagues exploited. He decided he would write a paper on their work, titled My Tumour and How I Solved It.
Initially Steinman wanted to undergo each treatment individually, so they could be independently assessed and provide better data.
“It was the weirdest experience,” remembered Ira Mellman, from Genentech, in an interview with the journal Nature. “Like we were having a lab meeting from the old days: talking about what experiments to do, what needed to be found out, how interesting it was, what you can and can’t do. It was a totally natural scientific discussion, except we were talking about his tumour.”
They persuaded him to use all the therapies at once. One vaccine stimulated the dendritic cells with specially tweaked tumour cells. Another pumped them full of his tumour RNA. A third exposed them to protein fragments from the surface of the cancer.
In early 2008 he was still alive – and he shouldn’t have been. He saw in 2009. Then 2010. But 2011 would be his last. When he died, the cancer was everywhere.
Cancer vaccines are, as Sahin admitted, alluringly simple. The immune system is anything but.
Christian Ottensmeier, professor of immuno-oncology at the University of Liverpool, has seen the field go through cycles of hope and despair before, and has himself worked on early stage research. The experience naturally builds scepticism. “These things have come in waves,” he says.
There is a lot that can go wrong when cherished ideas collide with the reality of the body. Dendritic cells, for instance, do indeed tell the body what to attack. They can also be used to tell it what not to attack. But Ottensmeier believes their time is coming. The reason is because of what happened next for Sahin and Toreci, and for the handful of others pursuing similar approaches.
By late 2019, not one of the mRNA companies had been successful. As BioNTech’s offerings entered small trials, there were mutterings among investors that the billions poured into mRNA research had yet to produce a successful therapeutic.
Then, in China, a bat got sick, a human got sick and everything changed. In January 2020 Sahin called a staff meeting and announced that their cancer vaccine company was going to become a coronavirus vaccine company. Or, at least, most of it was. No longer, to put it mildly, was there no successful mRNA therapeutic. The attention the coronavirus vaccine brought the company accelerated the technology, vindicated investors and highlighted the reason it existed at all: the search for a cancer treatment.
Thirteen years after Steinman rolled up his sleeve for his cancer vaccine, a small handful of patients did the same for BioNTech’s. Like Steinman, they also had pancreatic cancer. Like Steinman, they knew they should be dead within a year. Pancreatic cancer is a particularly terrible disease precisely because it is so good at beating the immune system, but out of 16 patients given BioNTech’s treatment, eight had an immune response and were cancer-free 18 months on. Among the other eight, six died or saw their cancer return.
Now a vaccine is being trialled in a far larger group, for bowel cancer. “Vaccines, I think,” says Ottensmeier, “are set to become the centrepiece of immunotherapy.”
Vaccines eradicated smallpox. They have almost eradicated polio. They created the post-Covid world. But cancer is wilier than a virus. Vaccines will not be “the” cure. They will, for some cancers, in some people in some circumstances, be a cure. Some patients will take them to stop cancers returning. Some will use them alongside other immunotherapies. Many will experience the full suite of cut, burn and poison first. Sometimes they may only buy time. Like Steinman, patients might see a few more springs than they expected. Do not underestimate, though, the value of buying time.
When Steinman died, his family told few people. Even by October 3, 2011, few scientists knew. That morning Claudia Steinman went downstairs to see her late husband’s phone blinking with a message. Still waking up, she idly picked it up to read it. A few seconds later she shouted up the stairs to her daughter Alexis: “Dad got the Nobel!” It remains the only modern posthumous Nobel prize.
The Times



To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout