Stress link to illness proved by new study
Scientists prove link between stress and falling ill and say nerve signals caused by stress can paralyse immune cells and stop them from fighting disease.

Australian scientists have proved the link between stress and falling ill, after discovering that nerve signals caused by stress can paralyse immune cells and stop them from fighting pathogens and even cancerous tumours.
In a world-first breakthrough, a Doherty Institute study has uncovered the link between stress and low immunity that many Australians already suspected — that the body’s immune cells stopped working during periods of increased fear and anxiety.
The head of the Peter Doherty Institute for Infection and Immunity Laboratory, Melbourne University professor Scott Mueller, who led the project, said his team was able to observe the impact of stress using an advanced imaging technique called intravital microscopy.
“We know anecdotally that when we are stressed, we are more likely to get sick, but exactly why this occurs has been difficult to define, until now,” he said.
“The imaging showed us that stress caused immune cells to stop moving, preventing them from protecting against disease.
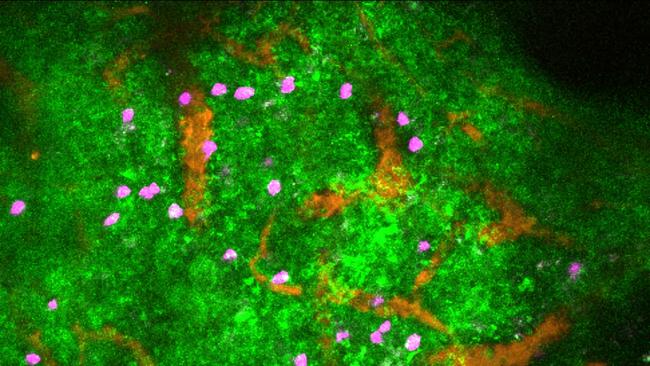
“Movement is central to how immune cells can get to the right parts of the body to mount an immune response against infections or tumours, so it was surprising to see that the stress signals had such a rapid and dramatic effect on how immune cells move around.”
Professor Mueller said the study, which measured nervous system signals called neurotransmitters, allowed his team to observe a drug-induced stress response in living mice, allowing them to make the world’s first link between stress and illness on a cellular level.
“It’s a microscope run by high-powered lasers,” he said. “We use the lasers to shine deep into the tissue and see the cells moving in the body.”
Professor Mueller said it wasn’t clear yet what kind of stressors — whether it was something like a shock from hearing life-changing news or ongoing psychological stress — had this impact on the neurotransmitters, only that there was a link.
“These neurotransmitters are needed just to keep us alive and to modulate heart flow and breathing,” he said. “When you’re stressed — the flight or fight response — your body produces a lot more of these, and it’s when the body releases more that the immune response is affected.
“We don’t know if it’s a sudden shock or other stresses at this stage; we don’t know what stressors affect the immune system in this way.”

He said the potential practical implementations of the findings were huge, with neurotransmitters already being used in medicine. “If a patient goes into a clinic undergoing septic shock, they’re treated with these neurotransmitters which is essential to restore blood pressure,” he said.
“Given what we’ve found there could be an ongoing impact with the nervous system. This is important knowledge translating into helping cancer patients who can be very stressed about this disease, and we know that stress makes cancer worse.
“There may now be a pathway that we can target to immune response to help treatment responses in cancer patients.”
The findings also had implications for new treatment pathways involving beta blockers, which are also already being used to treat serious diseases.
“Beta blockers block the neurotransmitter pathway and are used for people with heart disease and people with other conditions to alter these pathways,” he said.
“Some cancer patients if they take these beta blockers they may be better off with their disease.”







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout