Only real options are vaccination or risk death by Delta
Fourteen of the nation’s leading medical experts - including Nick Coatsworth and Ian Frazer - call on all adults to get any vaccine they can | READ THEIR OPEN LETTER

The most common question we are being asked each day as health professionals is: “What should I do about a vaccine?”
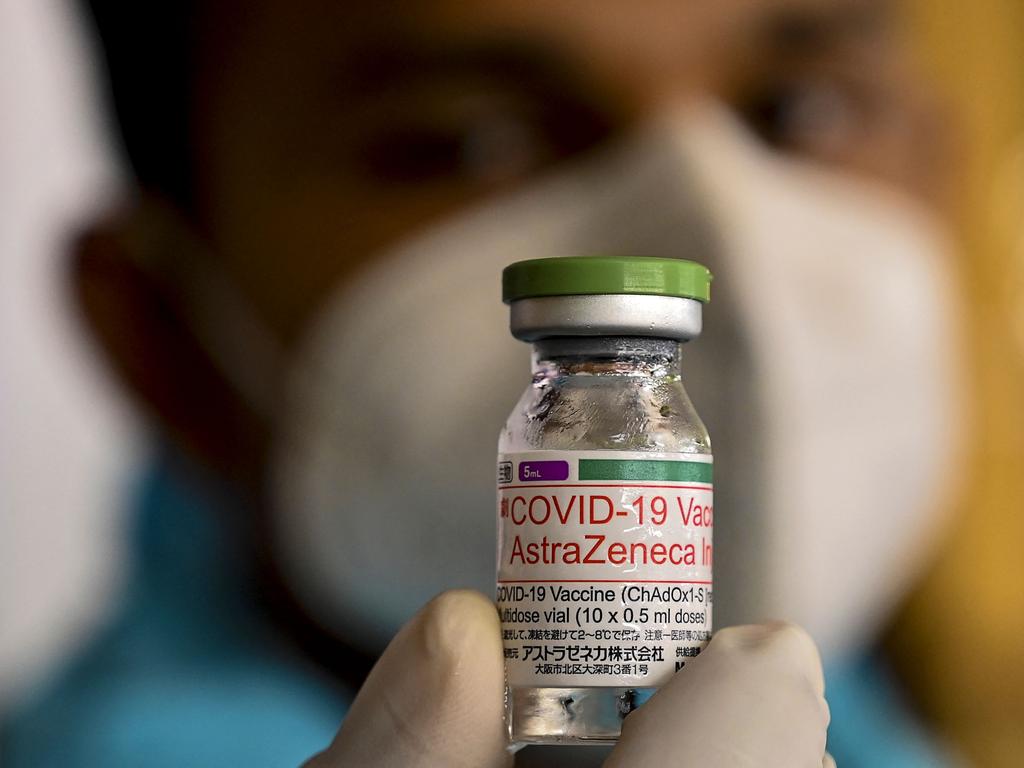
At present there are two Covid-19 vaccines available in Australia. Both are highly effective at preventing serious illness from Covid-19. Both have very rare side effects.
But, as we move into August, with NSW hospitals filling as a result of thousands of people infected with Covid-19, and cases emerging in Queensland and elsewhere, there are millions of unused doses of AstraZeneca vaccine sitting in GP surgeries and vaccination clinics.
In contrast, although supplies of the Pfizer vaccine are gradually increasing, there is insufficient supply to meet demand. Each day patients ask: “Should I wait for a Pfizer?”
The Delta variant of Covid-19 is highly infectious and appears to infect far more young people than earlier strains. It causes generally mild disease in vaccinated people, as evidenced in North America, Europe, Britain and vaccinated populations in Asia. Unvaccinated people are virtually the only ones who are dying of this strain.
The disease is rising in Australia. If it escapes into an unvaccinated population, it is possible that we could have thousands of people infected each day. Lockdowns are necessary to limit the number of new cases a day, to enable our health system to manage them, and to minimise the heavy toll Covid would otherwise inflict.
Through a combination of good management and good fortune, Australia has escaped the worst of the Covid pandemic. But we cannot, as a nation, continue to keep highly infectious strains of Covid at bay without major economic and social costs. Lockdowns alone cannot prevent the spread of the virus and they cause terrible stress and economic hardship.
Against that background, our strong recommendation to all Australians in an outbreak setting is to get a first dose of AstraZeneca or Pfizer vaccine as soon as possible, followed by a second dose as soon as possible. This is consistent with the latest Australian Technical Advisory Group on Immunisation advice. Do not wait for the Pfizer vaccine if the AstraZeneca vaccine is available to you.
AstraZeneca is an excellent vaccine that has already saved millions of lives and will save many more. Covid kills, and by the time you or someone you love is infected, hospitalised or in ICU it is too late.


Concerns in the community about AstraZeneca – and preference for Pfizer – fall into two main categories.
First is safety, and the commonly expressed concern by patients that the AstraZeneca vaccine is not safe because of a link to a rare blood-clotting syndrome. Second is efficacy, and the current broadly held perception by patients that Pfizer offers better protection.
In terms of safety, the side effect of the AstraZeneca vaccine, the blood-clotting syndrome called thrombosis thrombocytopenia syndrome is rare. For Australians over 50, the incidence of TTS following the AstraZeneca vaccine is about one in 50,000. In people under 50, the incidence is about one in 35,000. Death has occurred in about 5 per cent of people who had TTS, a less than one-in-a-million chance of dying as a result of vaccination. The low mortality rate compared with other countries is likely due to rapid implementation of improved diagnostic techniques and earlier effective treatments.
Without getting into the minute details of exact risk for people of different ages and acknowledging that risks are slightly higher in younger people, the risk of TTS-caused mortality following vaccination is extremely low for all age groups. Significantly lower, in fact, than many other well-accepted medical interventions and treatments.
The risk of death from Covid-19 in Australia, in contrast, is one in 35. While the risk of death is highest in older age groups, we are now seeing serious illness and death in unvaccinated young patients.
The risk, however, is also not all about simple survival. Between 10 and 30 per cent of people who contract Covid will suffer long-term health consequences, the seriousness of which is yet to be fully understood.
The related commonly asked safety question is whether people should have AstraZeneca if they have an existing health condition. “I have a heart condition so should I have Pfizer?” or “I had blood clots in the past so isn’t it dangerous for me to have AstraZeneca?” are frequent queries.
Blood-clotting experts have identified four rare health conditions that preclude people from vaccination with AstraZeneca: a previous history of cerebral venous thrombosis, abdominal vein thrombosis, heparin-induced thrombocytopenia or antiphospholipid antibody syndrome with blood clots.
But for all others (although excluding pregnant women) there are no pre-existing health conditions for which there is any evidence that should prevent them from having AstraZeneca vaccine. People with a heart condition, diabetes, a history of deep vein thrombosis, a history of cancer, and many other chronic or severe conditions can be reassured that based on real-world data from the hundreds of millions of AstraZeneca vaccine doses administered, they face no additional risks. There is no evidence the vaccine impacts fertility.
The advice for pregnant women has been updated and they are now advised to seek Pfizer vaccine if available. This is because there is less experience of AstraZeneca in pregnant women, not because there is evidence of increased risk. On the other hand, if pregnant women become infected with Covid-19, they are more likely than other women of the same age to have severe symptoms and need hospital admission.
In terms of effectiveness in preventing severe disease, both AstraZeneca and Pfizer have similar profiles against Delta. Delta presents a greater challenge than previous variants of Covid. People who have one dose of AstraZeneca or Pfizer gain 33 per cent protection against severe disease caused by Delta, less than the protection provided for earlier Covid variants. Two doses however, whether AstraZeneca or Pfizer, are both highly protective against severe disease.
Australia is at a critical point in the pandemic. In the past month we have had Covid lockdowns in NSW, Victoria, Queensland and South Australia. Vaccines offer our only pathway to safeguarding the health of the community, preventing unnecessary deaths, avoiding the financial and health costs of future prolonged lockdowns, and opening our country back to the world.
It is a phenomenal feat of human ingenuity and collaboration to have even one vaccine available so quickly after this new viral challenge arose. To get back to our normal lives, we need to make the most of every vial of every vaccine made – including AstraZeneca.
Bruce Robinson, endocrinologist, Royal North Shore Hospital
Nick Coatsworth, infectious disease and respiratory physician, Canberra Hospital
Mark Hertzberg, haematologist, Prince of Wales Hospital
Tony Cunningham, virologist, Westmead Institute for Medical Research
Michael Grigg, vascular surgeon, Box Hill Hospital
Vijay Roach, obstetrician and gynaecologist, Royal North Shore Hospital
Tania Sorrell, infectious disease physician, University of Sydney
Bernie Hudson, infectious disease physician, Royal North Shore Hospital
Steve Hambleton, general practitioner, Brisbane
Gemma Figtree, cardiologist, Royal North Shore Hospital
Danny Hsu, haematologist, Liverpool Hospital
Ian Frazer, clinical immunologist, University of Queensland
Lyn Gilbert, senior researcher, Marie Bashir Institute for Infectious Diseases and Biosecurity
Anthony Holley, intensive care specialist, Royal Brisbane and Women’s Hospital






To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout