Coronavirus: Three wise men crack the code, now to save the world
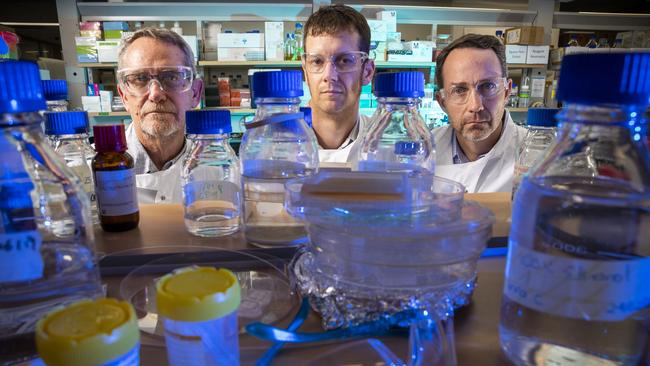
With millions of lives at stake, three Brisbane scientists believe they have come up with a COVID-19 vaccine that will work.

Day by day they’re edging closer to a vaccine for COVID-19, but there can be no cutting corners, no half-measures when millions of lives are at stake. In a very real sense, these three Brisbane scientists have the weight of the world on their shoulders.
Keith Chappell came up with the idea to hijack the virus’s own fearsome infectious properties with revolutionary “molecular clamp” technology, and since January he has worked around the clock with colleagues Paul Young, Trent Munro and Daniel Watterson to put it into a jab to inoculate the population.
After experimenting with 250 different formulations, they have settled on a candidate vaccine, S-Spike, and this is being tested on laboratory mice at the University of Queensland as a prelude to human trials by mid-year. There is every chance the team will be the first in the world to bring it to market.
“In terms of getting a vaccine that we think will work, we think we are already there,” said Dr Chappell, 38.
“But getting a vaccine that’s available for seven billion people on the planet means … we have to move to scale, and that’s a very different proposition.
“It’s all about how much risk we are willing to accept.”
He stressed he was talking about commercial risk, not jeopardising the safety and efficacy of the vaccine because that was non-negotiable.
Yet the scale of the unfolding crisis here and abroad calls for extraordinary steps to telescope into months the proving and development processes that typically take years for a new drug.
Leveraging the experience of Professor Munro, 44, in biotech in the US, they are already negotiating with regulators, including the federal government’s Therapeutic Goods Administration and the European Medical Association, to run the gauntlet of approvals while the finetuning continues in their lab and at the University of Melbourne’s Peter Doherty Institute for Infection and Immunity.
The UQ team met TGA officials on Friday to nut out how the dual-track approach would work.
As Dr Chappell revealed, walking The Weekend Australian through their progress in the cluttered labs in the Australian Institute for Bioengineering and Nanotechnology on UQ’s St Lucia campus, the vaccine was on track to be available by the end of the year, well ahead of the timetable flagged this week by Scott Morrison when he unveiled multi-billion-dollar funding packages for research and the public health response, and to underpin a flagging economy.
Hard decisions on the rollout were pending. “Do we produce a lot of the dose already, given the results we have got?” Dr Chappell asked rhetorically. “Or do we wait until after we have shown it works in the first group of people before we move to larger scale production?
“I think the size of this epidemic means that we need to bring manufacturing forward so that we are running the manufacture and the clinical trials in parallel so that the moment we have success in the clinic, we have doses that are ready to go.
“This will allow us to provide protection for the most vulnerable people in Australia — the elderly and all the hospital workers, because they are going to be overrun. These are the people who really need this insurance policy.”
Crucially, the researchers know with certainty that the vaccine works on coronavirus — not COVID-19, but its close relative, MERS, the lethal Middle East Respiratory Syndrome. With a fatality rate of 30 per cent, it is many times more dangerous than COVID-19, though thankfully far less contagious. Candidate vaccines for MERS and seasonal influenza using the molecular clamp had demonstrated powerful immune responses in animal studies before the new virus erupted out of China, said Professor Young, 64, head of UQ’s School of Chemistry and Molecular Biosciences.
“It’s a tried and tested model for influenza infection and what we showed was that our vaccine completely oblates virus growth in animals that were challenged, an extremely potent response,” he said.
“We don’t believe it is going to be any more complicated than with influenza, in fact it’s a little less complicated … because overall the coronaviruses don’t drift in their mutation as much as influenza does.”
Like most good ideas, the concept of the molecular clamp is deceptively simple. A virus is no more than a packet of malevolent genetic information that has one purpose in life: to find somewhere to lodge and replicate itself.
The surface of the COVID-19 virus bristles with so-called spike proteins, coiled like springs until they bind to a host cell.
The technology uses an ingenious lab-created polypeptide — a sequence of amino acids — to pin the spike protein in its tortile position so the body’s immune system can target it before the virus has a chance to activate. An adjuvant, or boosting agent, is added to the vaccine to stimulate the immune response.
The lightbulb lit up for Dr Chappell while he was completing post-doctoral studies in Madrid on the stabilisation of viral proteins. When he returned to UQ in 2011, where he had earned his PhD under the supervision of Professor Young, he realised that the molecular clamp could be used as a generic platform to provide immunity to different viruses, a kind of “plug and play” mechanism.
In addition to flu and MERS, it has been successfully tested in the lab on some of the world’s most deadly contagions, including SARS, Ebola, respiratory syncytial virus and Nipah, a cousin of Australia’s baffling Hendra virus transmitted from bats to horses then to people.
“All of these viruses have a very similar protein on the surface … assisting in the fusion of the viral membrane to the host cell membrane,” Professor Young said.
“They have a similar mechanism for their underpinning and we have shown that the clamp approach will work equivalently in each of them. Having said that, we need to adjust and modify for each one.”
The potential of the technology was recognised in 2018 by CEPI, the Oslo-based Coalition for Epidemic Preparedness Innovations that is headed by former federal health department boss Jane Halton and backed by the financial muscle of the Bill and Melinda Gates Foundation.
It pumped $14.7m into the molecular clamp program, one of three vaccine projects worldwide to be funded. The plan was for the UQ team to conduct a “stress test” next year to show it could produce a vaccine for an emergent pandemic agent within 16 weeks.
Instead, COVID-19 plunged the researchers and their augmented staff of 20 into an exhausting, real-world test of the fledgling technology.
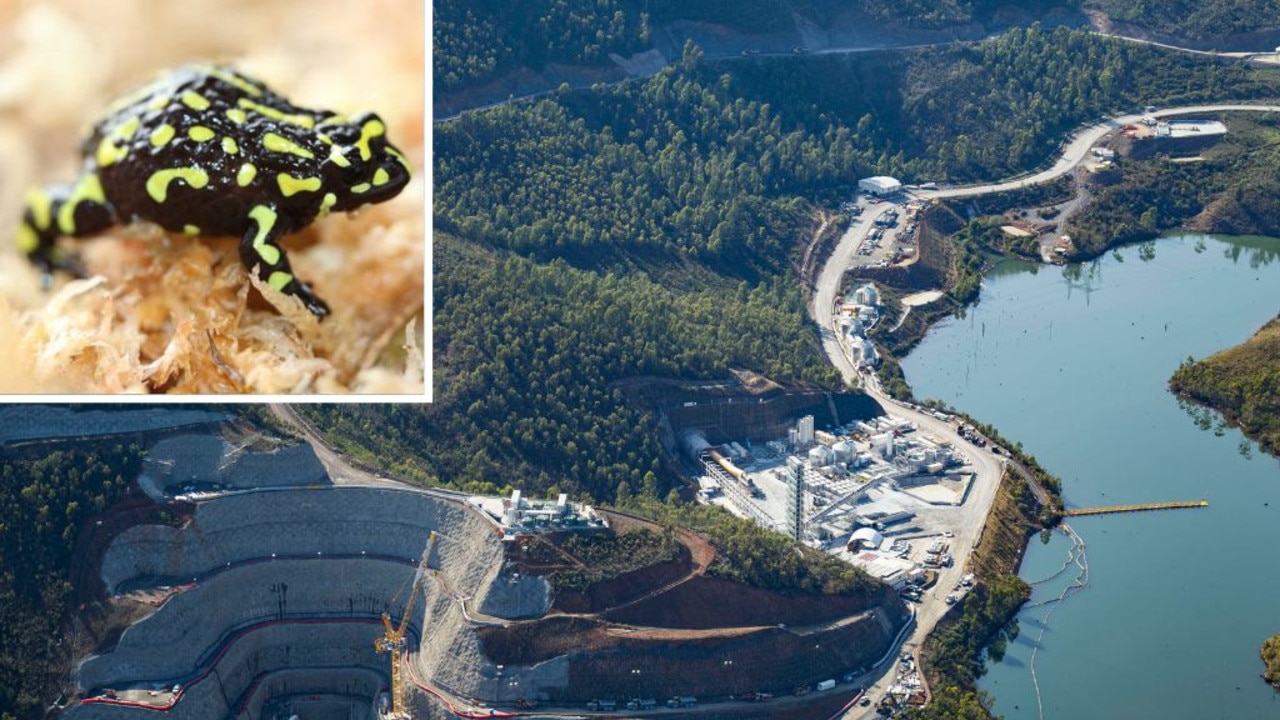
Vials of frozen Chinese hamster ovary cells seeded with the candidate vaccine have been sent to the CSIRO’s Clayton vaccine-making plant in Melbourne to pave the way for scaled-up production, while Big Pharma companies including Australia’s CSL-Seqirus and British multinational GlaxoSmithKline are on-board, offering their adjuvants.
Another group of scientists at the Doherty Institute was plotting antibody responses to the vaccine and identifying potential human immune markers to confirm its effectiveness, under the partnership between the University of Melbourne, University of Queensland and the nation’s premier science agency.
Further animal testing involving live coronavirus would be conducted at CSIRO’s Australian Animal Health Laboratory outside Geelong. The first results from the lab mice at UQ are due next week.
Scientists in China, Israel and the US are also scrambling to produce a vaccine, with American company and CEPI beneficiary Moderna Therapeutics considered to be best placed to deliver. For now.
While emphasising it was not a race — “we are keen for everyone to work on this and the prize is a viable vaccine, not who gets there first,” Professor Young said — the gains made by Moderna were early ones using a different process to target viral spike proteins with synthetic messenger RNA.
“With us, having optimised the protein process, we think we are in a better stage in terms of the vaccine-induced immune response,” he said.
Professor Munro, who had headed process development at US biotech firm Amgen before joining the UQ team last August, said the science of developing the vaccine was nearly complete, and the question was now how to get the drug into production.
This would cost between $20m and $30m.
“We would love to be able to do all the manufacturing here in Australia, to make the vaccine here, but that is going to be very, very difficult,” he said. “That whole sector has been eroded … even though companies like CSL-Seqirus have great manufacturing capabilities. We would just love to see more of that.”







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout