Two in three nursing home providers running at a loss
Nursing homes are in deep financial trouble, with 66 per cent of private providers operating at a loss and haemorrhaging an average $28 per resident each day.

Australia’s nursing homes are in deep financial trouble, with 66 per cent of private providers operating at a loss and their facilities haemorrhaging an average $28 per resident each day, new official data reveals.
The most comprehensive audit of aged care undertaken also finds nursing homes are spending an average $12.40 a day on food and ingredients for each resident, and the average hands-on care time provided in facilities sits at a little over three hours a day.
The inaugural Quarterly Financial Snapshot of the Aged Care Sector reveals for-profit and not-for-profit private providers, representing more than 90 per cent of all homes, returned a collective net loss before tax of $465.3m for the September 2022 quarter, off revenues of $5.3bn.

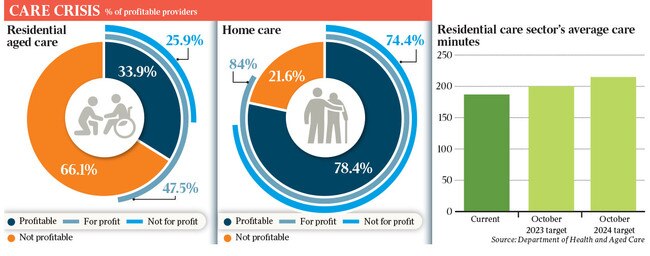
Just 34 per cent of private nursing home providers were running in the black, according to the report, which was based on new mandatory reporting requirements for providers. Almost half, 47 per cent, of for-profit residential aged-care providers were profitable compared with just one in four in the non-profit sector.
Local, state and territory government providers were not included in the financial data.
By contrast, 80 per cent of in-home aged-care service providers were running at a profit. “For-profit and not-for-profit home care providers returned a collective net profit before tax of $92.4m (off revenues of $1.28bn). This equates to a net profit before tax of $5 per care recipient per day,” the report said.
The perilous financial situation in the residential aged-care sector is a significant concern for Jim Chalmers as he prepares the May budget. Aged care is one of the federal government’s largest spending programs, with $27bn budgeted for in-home and residential care this financial year, rising to almost $35bn by 2025-26.
Recent funding boosts in the wake of the aged-care royal commission – including $3.2bn over four years to provide $10 per resident a day to improve the quality of care, and food, introduced by the Morrison government in 2021 – have not turned things around.
While the Albanese government committed a further $2.5bn over four years in last October’s budget to increase daily care minutes for nursing home residents, a key recommendation of the aged-care royal commission, providers say it doesn’t address the underlying unprofitability of their existing operations. Costs have risen rapidly driven by high inflation across the board.
The Treasurer must also find new money to fund a 15 per cent interim pay rise awarded by the Fair Work Commission to about 320,000 aged-care workers in November, as it was not accounted for in his October budget.
Industry estimates put the extra cost at about $1.9bn a year.
The FWC has yet to make a final ruling on the unions’ ongoing claim for a 25 per cent pay rise, and for it to apply to a greater range of non-direct care workers such as gardeners and cleaners, which would push wage costs even higher.
A submission in December by the government to split the pay rise into a 10 per cent hike on June 30 this year and a further 5 per cent in mid-2024 – a sign of the financial pressure the government is under – was rejected this week by the FWC.
Dr Chalmers has indicated he will find the extra funds to pay the additional 5 per cent, understood to be about $540m, from June.
His budget calculations around aged care are complicated by the fast-rising cost of another human services spending program, the $34bn-a-year National Disability Insurance Scheme.
NDIS Minister Bill Shorten is pressing to limit the pace of growth in the scheme with a crackdown on fraud and waste.
The new quarterly financial snapshot is published by the federal government in response to the aged-care royal commission’s call for greater transparency in the sector. Ninety-nine per cent of the 805 residential aged-care providers reported their figures, along with 96 per cent of the 924 homecare providers.
It provides information on financial performance including liquidity, care costs and care minutes provided, as well as food and nutrition.
Aged Care Minister Anika Wells said the snapshot was critical to support sustainability in the sector, but accepted it was under significant financial stress.
“You can’t improve what you can’t measure, which is why the Albanese government is committed to stronger reporting and oversight in aged care,” Ms Wells said. “The snapshot shows the strain a decade of inadequate funding from the Coalition has put on the aged-care sector.
“We’re certainly not shying away from the challenges ahead. We know there is much to be done in future-proofing aged care.”
The new financial data for residential aged care is even worse than recent industry estimates, which led analysts to warn of an “aged-care death spiral”.
A financial report in January by aged- care specialists StewartBrown for the September quarter, based on a survey of about 45 per cent of nursing homes, said losses were running at about $21.30 per resident a day, equating to annual losses of about $1.4bn. In September 2021 the same report put the losses at $7.30 per resident per bed, revealing the sector’s steep financial decline.
Tom Symondson, chief executive of peak provider advocacy group Aged and Community Care Providers Association, said the financial situation in residential aged care had been worsening for five years.
“The cost of care is going up drastically, the cost of wages is going up dramatically, inflation is driving up the cost of all manner of things in aged care, and funding simply hasn’t kept up with those increases for many years,” Mr Symondson said. “Facilities want to avoid at all costs delivering poor care, so their choice is to reduce the number of people they provide care to, or make a loss. It’s why we are seeing an increasing number of providers opting out of the sector altogether.”
Beyond the troubling financials, the snapshot reveals how much care time is being spent with residents, and how much money is being spent on food and nutrition. There were notable variations between for-profit and not-for-profit providers, as well as regional and city facilities.
While the median cost of food was $12.40, costs ranged from $11.70 per resident a day in for-profit metropolitan facilities to $16.60 in homes run by local, state or territory governments. Around 81c in every dollar was spent on fresh food and ingredients.
The report found the total care minutes per resident a day for the sector was 187 minutes. For-profit providers reported 179 minutes. The average care minutes comprised 34 minutes for registered nurses, 15 minutes for enrolled nurses and 138 minutes for personal care workers.
From October this year, it will become mandatory for providers to deliver an average of 200 care minutes per resident a day, including 40 minutes of registered nurse time.
This increases to 215 minutes from October 2024, including 44 minutes of registered nurse time.








To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout