Coronavirus: Nursing home death toll down by 1000
The number of deaths of nursing home residents has fallen by almost 1000 in the first seven months of 2020 compared with the year before.

The number of deaths of nursing home residents has fallen by almost 1000 in the first seven months of 2020 compared with the year before, even taking into account those who have died this year from coronavirus.
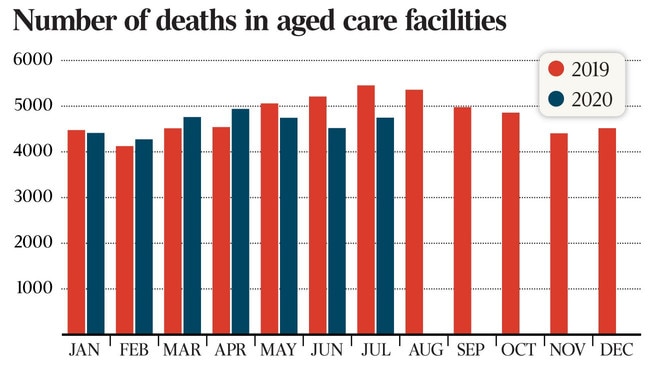
Overall, 32,398 nursing home residents have died in the year to July, unpublished Department of Health data reveals, compared with 33,383 in the first seven months of last year.
In particular the autumn and winter months of May, June and July have experienced significant year-on-year falls. In July last year, 5455 nursing home residents died, compared with 4747 in July this year.
While most of the 505 COVID-19 related deaths in Victorian aged-care facilities to date were reported in August, the Andrews government this week added more than 80 deaths that occurred in July or August. Those deaths were reclassified after inconsistencies between the way state and federal authorities report them.
Twenty-nine nursing home residents died in earlier outbreaks in NSW, including 17 at Newmarch House.
The fall in nursing home deaths across the nation is likely the result of increased influenza immunisation rates in the community and infection control protocols introduced during the pandemic, the department said.
But Joseph Ibrahim, head of the health law and ageing research unit at Monash University’s department of forensic medicine, questioned what it said about past practice if better infection control and lower flu rates were behind the improved numbers.
“If lower death rates were a secondary benefit of increased control measures, it raises the question whether a large number of preventable deaths have been occurring for years in aged care,” Professor Ibrahim said.
“We already know from research studies that aged care did not have optimal infection control measures.”
He said a greater public focus on aged care might have led to better care for residents, “again an indictment on the system as preventable deaths must have been occurring on a larger scale than we previously thought”.
Overall, about 240,000 Australians use residential aged care each year, and 55,000 to 60,000 die, about 40 per cent of all yearly deaths across the nation.
The recent spate of COVID-19 related deaths in nursing homes has ramped up pressure on the Morrison government for its handling of the sector during the pandemic. The Senate this week censured Aged Care Minister Richard Colbeck over his performance and the federal opposition focused on aged-care issues almost exclusively in question time during the past fortnight.
Last month the aged-care royal commission’s counsel assisting Peter Rozen offered a savage critique of the federal government’s management of the risk of COVID-19 in aged care, saying it did not have a specific plan to manage the crisis even though the disease’s impact on vulnerable nursing home residents could have been foreseen.
Scott Morrison has strongly rejected that assessment and defended his minister.
With the death toll from Victorian nursing homes continuing to mount, Senator Colbeck and Health Minister Greg Hunt last week announced a $245m funding package for residential aged-care facilities to fund and support infection control capability, including through an on-site clinical lead.
Kathy Eagar, director of the Australian Health Services Research Institute at the University of Wollongong, said she was shocked to learn this year that many homes didn’t have anyone responsible for infection control and training was “patchy at best”.
“Infection control should be core business in aged care, especially because flu and gastro outbreaks are so common.
“The silver lining from COVID may be the infection control systems that the commonwealth has finally required homes to put in place. They will not only prevent more COVID deaths but also deaths from flu and other infections,” Professor Eagar said.
Infectious disease expert Sanjaya Senanayake said while it was just two years of data, lower levels of flu in the community were a likely reason for fewer deaths in residential aged care.
“Overall the large reduction in flu notifications this year compared to last year is probably at least partly due to the measures brought in to address COVID throughout the community, including in schools, although flu numbers will vary year to year,” he said.
Dr Senanayake said nursing home residents might have been saved by a greater take-up of the flu vaccine across the broader community, and better physical distancing and hygiene control regimens in place for COVID-19.
“Possible explanations could be … staff and visitors adhering to physical distancing where possible, good hand hygiene, not mixing with others when sick,” Dr Senanayake said.








To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout