Aged and confused over care federal intervention in Victoria
Victoria’s aged-care COVID crisis is creating distress for residents and their families, with carers also revealing they feel unsafe.

The federal government’s handling of Victoria’s escalating aged-care COVID crisis, including its emergency response and plan to deal with the “cross infection” threat from carers working at more than one facility, is creating distress for residents and their families, leaving nursing home providers confused and making carers feel unsafe.
A government-ordered intervention last week at the Melbourne nursing home at the centre of Victoria’s worst aged-care coronavirus outbreak, St Basil’s Homes for the Aged, resulted in some residents being left without food and lying in soiled sheets.
Nursing home providers said that nine days after Aged Care Minister Richard Colbeck announced a new scheme to ensure carers weren’t putting residents at greater risk of COVID-19 by working in more than one home, they were still unclear about key details of the scheme, and workers are still engaged at multiple homes.
A survey of 1000 carers by their union found two-thirds felt unprepared to deal with a coronavirus outbreak and almost one-third said they had received no additional training in COVID-19 safety measures or how to use personal protective equipment.
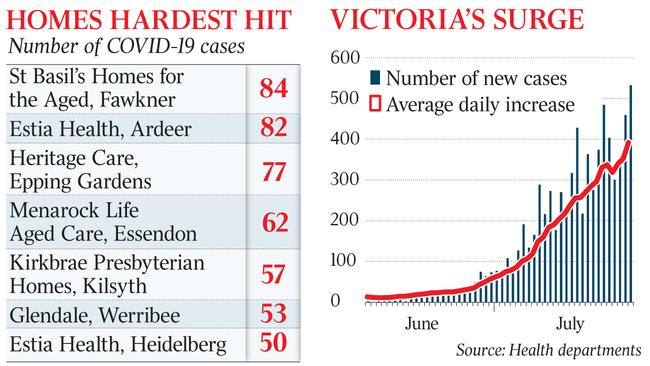
Victoria’s aged-care system, virtually clear of coronavirus just three weeks ago, now has 683 active cases across 61 sites, up by more than 120 in a single day. Another five residents of aged-care homes died on Monday, bringing the total to 35 during the COVID second wave. Aged-care deaths have made up 60 per cent of all coronavirus-related deaths in Victoria since July 5.
Overall, there were 549 new cases recorded across the country on Monday, the single largest daily number and a figure described by Deputy Chief Medical Officer Michael Kidd as “very concerning”. Victoria accounted for 532.
“The tragedy of COVID-19 is that we know, with the number of infections we’ve seen today, that there will be further deaths in the days ahead,“ Professor Kidd said.
St Basil’s, a wholly owned charity of the Greek Orthodox Archdiocese in Australia and regulated by the federal government, has been linked to 84 cases of COVID-19, which members of Victoria’s public health team blamed on reluctance from management to allow an intervention.
At the request of the Victorian government, the commonwealth stepped in last Wednesday morning. It replaced regular St Basil’s staff with agency workers from health services company Aspen Medical. The Australian has been told by multiple sources that the staff provided were junior nursing graduates so unprepared for the role some residents were left without food and others were abandoned in soiled beds. There was also no proper handover and new staff were not aware of the location of keys to medicine cabinets.
The issues led to a second intervention late on Thursday by the state government, which sent in a dozen registered nurses.
The Australian understands the Andrews government has raised concerns over “clinical risks” at St Basil’s with federal counterparts. An Aspen Medical spokesman referred The Australian to the Department of Health for comment. The department did not respond.
Professor Kidd said roughly 5 per cent of all COVID-19 cases in Victoria since April could be linked to nursing home residents, with a further 4 per cent stemming from infected staff working at those facilities.
Besides St Basil’s, there are 82 cases at Estia Health in Ardeer, 77 at Epping Gardens Aged Care, 62 at Menarock Aged Care in Essendon, Kirkbrae Presbyterian Homes in Kilsyth has 57 cases linked to it and 53 are associated with Glendale Aged Care in Werribee.
Listed provider Estia risks having its federal funding revoked after it was served a “notice to agree” from the Aged Care Quality and Safety Commission following coronavirus outbreaks at two of its nursing homes in Melbourne.
Senator Colbeck said the rise in aged-care cases had been sudden.
“Three weeks ago we had four facilities where we had residents who had recovered from the virus and we were basically waiting for their isolation period to clear before we declared them COVID-free,” he said. “This circumstance has occurred in three weeks.”
As the numbers continued to rise, Senator Colbeck faced an escalating dispute with nursing home providers over how to ensure carers weren’t putting residents at greater risk of COVID-19 by working in more than one home.
Providers said they remained unclear about key details of a scheme announced by the government nine days ago.
“Aged-care peak organisations, providers and staff are still waiting to see exactly how this support will be provided so they can make appropriately informed decisions,” said Leading Aged Services Australia general manager of policy and advocacy Tim Hicks.
He said that workers were still turning up for work at more than one facility.
“Providers are doing their utmost to reduce staff movement, while ensuring that workers are not disadvantaged, but the top priority will always be to fill shifts to ensure that residents receive the care they need,” Mr Hicks said.
Senator Colbeck was adamant providers should have started rostering to ensure workers were at one nursing home only. “Aged-care providers were updated on the commitment by the commonwealth to support the program over the weekend,” he said.
A United Workers Union survey of 1000 aged-care workers found that two thirds of those interviewed said they did not feel very prepared to deal with a coronavirus outbreak.
Union director Carolyn Smith said the results confirmed workers felt untrained and unsafe during the pandemic.
Scott Morrison defended the government’s response on Monday and said the commonwealth had been taking action “for weeks and weeks”.
The Prime Minister said strong initiatives had been taken, such as training those working in aged care in infection control practises as well as supplying PPE equipment.






To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout