Is this a big enough shot in the arm for ailing Medicare system?
Incentive to bulk bill those in need has been tripled, but there’s no guarantee GPs will do so.

The cherished national institution of Medicare is synonymous for most Australians with the idea of universal healthcare.
But in the past year, as millions were told by their local doctor that their GP visits would no longer be bulk-billed, the denial of free primary healthcare came as an affront and a shock.
Many of those who could afford to pay were outraged to have to do so, but for those who could not afford to, the situation was critical as many thousands of doctors insisted they had little option but to charge gap fees even to pensioners and children, such was the serious erosion in the Medicare rebate and the rising costs of running a practice.
The consequence was that some of the most vulnerable people in the country could no longer afford to see a general practitioner at all – an unacceptable reality that no government could allow to continue, least of all a Labor government that had declared it had “no higher priority” than saving Medicare.
The Albanese government’s response to the immediate crisis in general practice was a $3.5bn policy that aimed to shore up access to bulk billing for 11 million children, pensioners and other welfare recipients.
This week’s federal budget tripled the incentive paid to doctors to bulk-bill such patients. In metropolitan areas the incentive payment will rise from $6.60 to $20.65, bringing the total Medicare allocation that will flow to doctors to about $60 for a 20-minute consultation for eligible patients. That sum will be higher in disadvantaged areas and the regions, peaking at a bulk-billing incentive alone of $39.65 in the most remote areas of Australia.
Another $2.2bn is being spent on expanding multidisciplinary care with the introduction of block funding to clinics to employ more nurses and allied health staff, upgrading digital systems, building more urgent care clinics, and other initiatives to strengthen a 40-year-old ailing Medicare system.
It’s just the beginning of a long-term project of reform that in time will include an inevitable overhaul of the Medicare Benefits Schedule to enable a much wider array of healthcare professionals to directly bill Medicare as nurses, pharmacists and paramedics move to work to their full scope of practice within a primary care setting to meet the significant needs of a population that is ageing and experiencing more chronic illness.
Structural reforms are long overdue, but the reality is that in the wake of this budget, many millions of Australians will continue to face average $40 gap fees each time they see their GP, often waiting many days or weeks for an appointment.
And despite the welcome injection of funds into incentivising doctors to bulk-bill those who need it most, there are no guarantees doctors will in fact do so everywhere in the country.
Given all of this, does universal healthcare in fact exist in modern Australia? Despite Medicare, did it ever exist at all?
Answering such a question is fundamental to tempering the expectations of the population as to what level of healthcare they can reasonably expect the state to provide and to what extent they should be asked to pay for it themselves. Pitching where it stands on this public-private policy mix, which has shifted over decades from a universal health insurance scheme that paid the vast bulk of Australians’ healthcare costs under Gough Whitlam’s Medibank, to John Howard’s characterisation of Medicare as fundamentally a safety net for those who could not afford private insurance.
In assessing the question of Australians’ current access to universal healthcare, author and academic James Gillespie points to the second reading of the Medicare bill delivered by Bob Hawke’s health minister, Neal Blewett, in 1983, which stated there should be “the same entitlement to basic medical benefits and treatment in a public hospital to every Australian resident regardless of income”.
“In a society as wealthy as ours there should not be people putting off treatment because they cannot afford the bills,” Blewett said. “Basic healthcare should be the right of every Australian.”

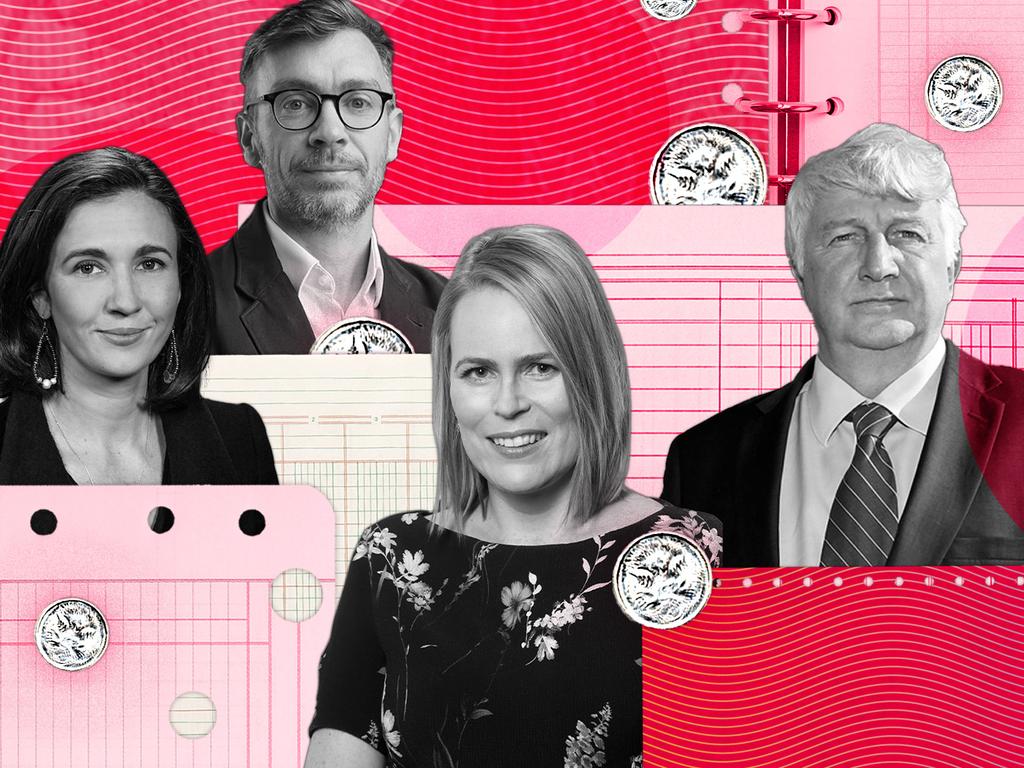
Against this bedrock position, Medicare is failing in its original purpose, says Gillespie, a honorary associate professor in the Menzies Centre for Health Policy and at the University of Sydney’s school of public health.
“I think there’s been a general erosion of each of those principles,” he says. “The co-payments in particular have increased enormously. Part of the problem is that we’ve had a long erosion of general practice. In the Blewett model, general practice was the gatekeeper. You went to the GP first, and preferably you paid nothing. But we’ve seen a steady erosion of bulk billing while the specialists have pumped up their fees. And so the relative position of GPs has declined as against the rest of medicine. GPs have been very slow to react, but when the reality finally sinks in, you get a quite a strong reaction, some of which is just early retirement for many doctors.”
Macquarie University Centre for the Health Economy director Henry Cutler says the concept of entitlement to free healthcare that is so deeply embedded in the psyche of many Australians was never actually matched in Medicare’s structure or policy.
“In terms of universal healthcare, I think that’s a bit of a misnomer because we’ve never really had universal healthcare,” Cutler says. “What we have had is universal health insurance where everyone has access to some form of government subsidy related to accessing healthcare.
“If everyone was bulk-billed, and no one was charged a co-payment, then we would have universal healthcare because no matter whether you earn $1m a year or $100 a year, you would still be bulk-billed. But we’ve never had that.
“Universal healthcare is really about being able to access care, regardless of income or regardless of where you live.”

One of the vexing issues facing governments attempting to increase equity and access in healthcare is that whatever the incentives or rebates they provide from the public purse, they are not in control of whether bulk billing will ultimately be provided to those who need it most. That’s the biggest risk with Labor’s $3.5bn bulk-billing incentives centrepiece policy.
“The way Medicare is structured means that the funds allocated to patients are funnelled through providers,” health policy analyst Jennifer Doggett says.
“So it means that you’re only funding services where providers choose to provide them to the people they choose to provide them to.
“There’s always going to be a disconnect between what the providers choose to do and what the greatest needs are in the community, and that sort of gap is where you get this undermining of universality.”
Former federal deputy chief medical officer Nick Coatsworth also is concerned at the prospect that doctors will not respond to the incentives and reinstate bulk billing on a large scale.
He welcomes the bulk-billing incentives policy as a positive response to the “significant issues of affordability” that undermined the fundamental basis of Medicare “to the point where we almost can’t say we have universal healthcare”.
But Coatsworth says that for policies aimed at restoring access to healthcare to be effective, they must be accompanied by greater regulation.
“Very few businesses have unfettered access to the Treasury coffers like doctors do,” he says. “So you can’t on one hand say you need to give us more subsidy and on the other hand claim to be a private business. That is what general practice does.
“This is the problem across Medicare, and it’s a problem across the NDIS, where you have provider-driven demand but there’s no certainty and no regulation about who should get bulk billing and who shouldn’t. You’ll get much less value in terms of bulk-billing increases unless you put some regulation behind increased subsidies.”
Cutler agrees there are problems with a “quasi means-testing arrangement that’s decided on by GPs rather than the government” which has been further entrenched by greatly expanded bulk-billing incentives.
“What our current system has is unfit for future needs of patients,” Cutler says.
“First of all, there needs to be efficiency improvements in the healthcare system. If they are going to be handing out more money, it needs to be within a framework of improving efficiency and effectiveness.
“We’ve got this push at the moment towards value-based healthcare and potentially value-based payments. And if that requires large-scale reform, then the government needs to look at how they can do that.
“That basically upsets the apple cart for business models that have been embedded for decades based on fee-for-service. The government has lots of opportunity to push reform forward and make efficiency No.1 because we just can’t keep spending.”







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout