Changing the rules to save men’s lives from prostate cancer
An urgent push is on to update testing guidelines for the most commonly diagnosed form of cancer: “If your doctor is not doing this test, then they’re taking away your right to know — and potentially live.’

When Chris Morley hears public health experts pronounce that most men die with prostate cancer rather than from it, it infuriates him. The 51-year-old former truck driver has metastatic prostate cancer and at best has only a few years to live.
Although it’s true that some men live long lives with prostate cancer they never knew they had, for the men whose cancers have already spread beyond the prostate by the time they are detected it is a devastating diagnosis and an exceptionally cruel disease.
“If my cancer had been detected earlier I would at least be in a better position than I am now,” Morley says. “If your doctor is not doing PSA tests then they’re actually taking away your right to know and potentially your right to life.”
Saving the lives of men such as Morley – more than 3,507 men like him die from prostate cancer every year – is the mission of the Prostate Cancer Foundation of Australia, which is leading work to update national clinical practice guidelines on prostate-specific antigen testing that date from 2016.
Read more

Chemical castration: the emasculating effects of prostate cancer treatment

If PSA testing was standard, my Dad might be alive today

‘Outdated’ cancer screening guide review
World-first trial for cancer sufferers

Men facing a deadly prostate cancer wave

Rule changes that could save men from an exceptionally cruel fate
Prostate cancer is the most commonly diagnosed cancer in Australia, with 24,217 men diagnosed last year and nine men dying every day from the disease. Five-year survival rates have improved from 60 per cent 30 years ago to 95 per cent now, but the number of men diagnosed in their 60s and 70s with advanced metastatic disease is significant, driving a push to review testing protocols taking into account evidence of the latest diagnostic and treatment practices that has radically changed the equation on PSA testing.
“The existing guidelines were based on evidence which has changed profoundly in the last few years,” says Jeff Dunn, who will serve as chief investigator and chairman of the guideline review steering committee.
“There have been major breakthroughs in technologies in relation to imaging and screening techniques. There have been magnificent breakthroughs in the way in which active surveillance is handled for men with early stage cancers, whereas years ago too many of those men were being treated.
“And the existing guidelines have never been uniformly applied. They were never accompanied by a companion set of consumer guidelines and a public education or awareness program. So there was never a serious attempt to get them embedded in our health and welfare system. The vast majority of men have got no idea what the guidelines say.”
This low awareness of screening guidelines among men has been accompanied by widespread variance in practice among GPs in recommending and ordering PSA testing. While many men over 50 are routinely screened, many others complain of being refused testing by doctors who say they don’t need it.
The Royal Australian College of General Practitioners finally is working to bring its own guidelines – which place the onus on men to request testing – into line with the National Health and Medical Research Council-endorsed 2016 national clinical practice recommendations, to the relief of urologists such as Mark Frydenberg, who specialises in urologic oncology and cancer surgery.
“We definitely as urologists see this, where patients have come to us saying, ‘Well, you know, the GP never mentioned PSA testing to us. We heard from a friend about it, then we had to go back and really ask for it.’
“But what is worse still is that even when patients asked to be tested, anecdotally, they were told, ‘Well, you’re going to come to more harm than good’, without necessarily going into a proper explanation about the possible benefits that they could get from PSA testing. And sadly, when we see people further down the track, and they’ve got advanced, incurable disease when it could have been picked up earlier, obviously that’s a bit of a tragedy.”
Population-based screening is not recommended for prostate cancer because the evidence indicates that not enough lives would be saved compared with the harms associated with overdiagnosis. But there’s now a push to extend the recommended age of testing to 79, strengthen the testing recommendations for those with family history and potentially shorten the recommended duration between tests to yearly. Such changes would result in a big increase in PSA testing and it has opened up a fresh debate over overdiagnosis and the extent to which changes in urological practice and diagnosis have ameliorated those risks.
Research led by Griffith University school of medicine researcher Thanya Pathirana from 2019 indicated that 41 per cent of prostate cancers in Australia were overdiagnosed. In the past, those diagnosed were often operated on and treated even for low-risk cancers. But changes in diagnostics and reductions in unnecessary treatment have significantly reduced the harms associated with wider PSA testing, with advocates of more screening arguing the debate has shifted firmly in favour of the benefits.
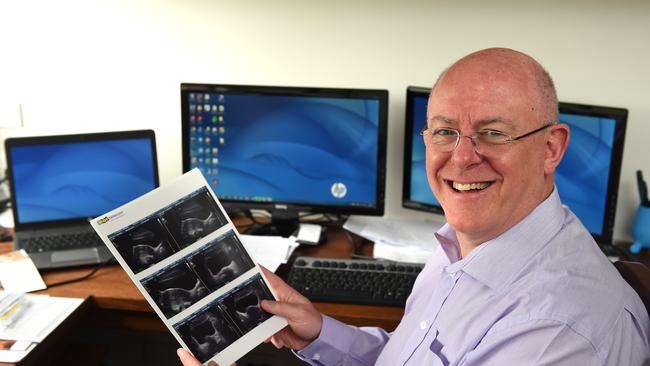
“The psychological impact of raised PSA and overdiagnosis has been greatly mitigated and frankly, compared to the impact of a late diagnosis, pales into insignificance,” says urologist Peter Heathcote, who sits on the board of PCFA and has been raising concerns at recent increases in the number of men being diagnosed with high to very high-risk forms of prostate cancer.
Advocates of expanded testing say overdiagnosis of prostate cancer due to PSA testing has reduced largely because multiparametric MRI is now listed on the Medicare Benefits Schedule for use in the diagnosis of prostate cancer.
The use of MRI also means many men avoid invasive biopsies. When biopsies are done, the method has changed so men no longer risk infections. The use of MRI also has had implications for treatment, with men identified as having low-risk cancers routinely placed on active surveillance rather than undergoing surgery or radiation therapy. The numbers of men on active surveillance, where the cancer is monitored six-monthly but not treated unless it grows, increased from 34 per cent in 2009 to 71 per cent in 2018. There has been a corresponding decline in surgery among men with low-risk cancers, from 39 per cent in 2015 to 24 per cent in latest figures.
The research collaboration for reducing overdiagnosis and overtreatment, Wiser Healthcare, does not believe there is yet sufficient evidence that the use of MRI has reduced overdiagnosis. “The impact of MRI on long-term outcomes of prostate cancer incidence, mortality and complications of treatment remains uncertain,” researcher Kristen Pickles says on behalf of the group.
“There is some emerging evidence suggesting that MRI could save men from unnecessary biopsy and increase detection of clinically significant cancers, and overtreatment may decrease with more men being placed on active surveillance. However, we know that asymptomatic men are impacted when they receive a diagnosis of, and are labelled with, prostate cancer. Active surveillance has its own harms and you can be on active surveillance but still could have been overdiagnosed.”
PCFA chief executive Anne Savage says the ultimate goal of the testing review is to catch more prostate cancers early, and any anxiety associated with active surveillance for men is outweighed by the pressing need to save lives.
Currently, a concerning 30 per cent of men aged 65 to 69 have high-risk or metastatic disease by the time they are diagnosed, and that figure is 41 per cent for men aged 70 to 74 and 60 per cent for those over 75. “Ultimately our aim here is to improve survival to reduce avoidable deaths from a disease which is eminently treatable if we can detect it before it spreads,” Savage says.
The University of Melbourne Herman chair of primary care cancer research Jon Emery is not convinced more screening saves many lives. He cites a 2018 meta-analysis of international prostate cancer trials that indicates only one to two men would avoid dying from prostate cancer for every 1000 men who undertook a PSA test, and another two men would avoid presenting with metastatic disease.
“From a public health point of view, the benefits don’t really clearly outweigh the harms,” Emery says. “We’re still in that place where we know that there’s a potentially small reduction in deaths from early detection through PSA testing.
“We’re still left with having to try and leave it for individual men to make what is quite a complicated decision, thinking about how they perceive this balance between early detection of cancer but then facing the potential consequences of treatment.”
Interpretation of the research is hotly contested, with Heathcote pointing to the authoritative European Randomized study of Screening for Prostate Cancer findings, which showed a 21 per cent reduction in prostate cancer specific mortality among men screened compared to controls after 11 years. The Swedish arm of that study indicated 293 men needed to be screened and 12 diagnosed to prevent one death.
Dunn says that even if only two lives are saved from PSA testing 1000 men, “that’s a pretty good day for those two men”.


“If there are still some areas of controversy, let’s encapsulate those and deal with them in the guidelines,” he says.
“We won’t answer the question if we keep saying it’s too hard and it’s a controversy. We’ve got to move past that. We’ve got to change the narrative. The dial has shifted, we are not where we were seven or eight years ago, we’ve got data from larger international trials coming in which we didn’t have six years ago, we’ve got so many more technologies in relation to imaging and screening, we’ve got changes of clinical practice. It’s an entirely different environment.”
As the review’s steering committee prepares to analyse and debate the evidence, many men are simply seeking clear guidance.
Psycho-oncologist Suzanne Chambers, author of Facing the Tiger: A Survivorship Guide for Men with Prostate Cancer and Their Partners, says for many of the hundreds of men she has counselled, the answers are already clear.
“I would have to say that of the men that I talk to, the ones that have found the prostate cancer early that is localised and when they have the opportunity to have treatment that is aiming for cure, they are almost all very relieved that they had that opportunity,” Chambers says.
“When I see a man with advanced disease who has not been tested, I fully understand why he feels angry. And I’ve seen many angry men. I’m devastated for them frankly.”
Morley is not sure whether he will be alive when the new guidelines are decided, likely to be a year away. But he wants the steering committee to keep one thing firmly in mind.
“Everyone has a right to life,” he says. “You might say: ‘We’re not going to test you because you don’t need it.’ Well, you’re not going to know who needs it unless you test.”


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout