Multiple myeloma drug subsidised after treatment costs ballooned
A newly subsidised immunotherapy for multiple myeloma presents the first chance for some patients to access such treatment.
It’s one of the few cancers still considered incurable, and those diagnosed with multiple myeloma will likely die from the disease, doctors say, but one of the scarce treatments available has now been made more affordable.
Multiple myeloma forms in blood plasma cells within bone marrow, affecting 2000 Australians a year. About 1500 of those are ineligible for stem cell transplantation – the standard treatment.
Australia’s record in treating the disease appears to be among the worst in the world, and one professor expert in the disease accuses authorities of squabbling over money while patients languish.
The Pharmaceutical Benefits Scheme approved the drug daratumumab on Thursday, providing a more affordable immunotherapy option for those ineligible for transplants or whose cancer is treatment-resistant. It is the first new treatment to be readily available for multiple myeloma in more than a decade despite progress abroad.
Patient Andrew Marks, who previously paid $400,000 for the drug, urged more timely consideration for cancer patients.
“It would be highly desirable if, in the future, some way could be found whereby drugs could be made available to cancer patients ahead of PBS approval, because for some cancer patients, they only get one chance and by the time approval comes through, it’s often too late,” he said.
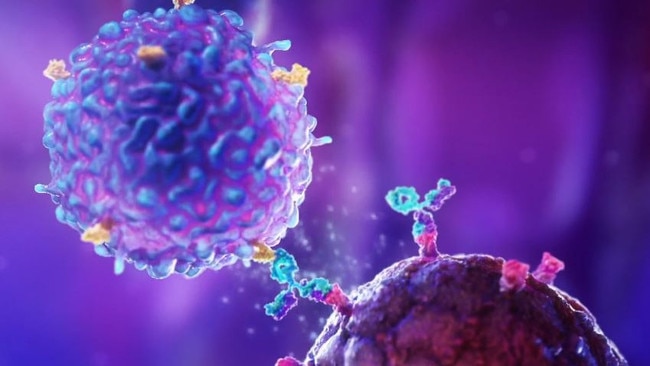
Immunotherapies train the patient’s immune system to identify and kill cancer cells, and can be applied in combination with chemotherapy and radiotherapy.

Alfred Hospital haematologist Andrew Spencer pioneered the national database used to track the prognoses and outcomes of multiple myeloma patients.
While glad to see daratumumab accessible for patients who have suffered cancer relapses, he argued protracted negotiations between government and pharmaceutical corporations were keeping treatments inaccessible, saying preventing access for patients who were eligible for stem cell transplants would cause suffering.
“A lot of what we do is about how to prolong longevity for patients with myeloma. It’s a very complex disorder and is one of the few cancers which would still be considered incurable. There’s not many, but it’s one of them,” Professor Spencer said. “If you get it, it’s highly likely you will die from it.
“It’s got this recurring clinical pattern, the natural history of the disease, and each time that it comes back, it tends to be more drug-resistant.”
Multiple myeloma is a disease of “attrition”, Professor Spencer said, with each round of relapse narrowing treatment prospects and hurting both the health and the hip pocket of patients.
“It’s a very costly cancer,” he said. “It’s actually a multi-system disorder … Not only do you have the primary disease to deal with, you’ve got all the comorbidities that are associated with it.
“For every month that these government bodies delay access to treatment, people are dying … I don’t think they get that while they’re squabbling over money there’s people at the end of the line … It just comes down to an accounting exercise.”
The lag in new treatments available is visible in Australia’s death rates for multiple myeloma. A 2022 Oxford Academic study placed the multiple myeloma mortality rate at 1.75 per 100,000 people in Australia and New Zealand, ranking worse than the Caribbean and anywhere in Asia or the Americas.
Daratumumab was previously approved for use in 38 countries. It extends median survival time by 26 months from 5.3 to 7.5 years.

Oncologists shy away from providing stem cell transplants to patients over 70, again reducing treatment options for patients whose cancer struggle has extended into their later life.
Former lawyer Mr Marks, 71, was diagnosed with multiple myeloma a decade ago and paid $400,000 for daratumumab under the brand name Darzalex before it was subsidised, eventually garnering compassionate access from producer Johnson & Johnson.
“I was very possibly the first Australian patient outside of clinical trials to access the drug. I required a special TGA approval. I was in a very fortunate position that I was able to fund it. That is exceptionally rare,” Mr Marks said.
“It’s a game-changer because the treatments do not make you sick, unlike treatments for other cancers.”
First diagnosed in September 2015, he relapsed a month later and was given 18 months to live, cycling through stem cell transplantation and other treatments until landing on daratumumab.
“It was a very big leap of faith, but there wasn’t any other leap that was readily available,” Mr Marks said.
“It is very unfair that some people are denied the best options because of financial circumstances, and it’s always been my wish that everyone could be in the same fortunate boat as I have been in.”








To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout