Coronavirus: Telehealth expands in Australia
Medicare funded telehealth is up and running in Australia, but there is confusion and teething problems as its availability expands.

Medicare funded telehealth is up and running in Australia, but there is confusion and teething problems as its availability expands. The new system lets patients have remote video and phone consultation with GPs or other health practitioners, and for it to be bulk billed to Medicare.
The Department of Health told The Australian that new Medicare telehealth items have been used to deliver more than one million services to almost 850,000 patients since March 13.
The department has published a broad list of consultation types that are funded. As well as GPs, there are social workers, psychologists, speech pathologists, pregnancy support, consultant physicians and mental health practitioners offering specified services.
Not all arrangements are in place. For one, medical associations want the government to make Medicare payments available for private consultations billed above the standard fee, so that they won’t be forced to bulk bill and lose income.
Former Australian Medical Association president Kerryn Phelps said big strides have been made in rolling out the system. The government has “expanded significantly” the Medicare mental health item numbers for teleconferencing and there were increases in the incentive for bulk billing telehealth conferences from $6 to $13.
MORE FROM CHRIS GRIFFITH: Reduce risks and Skype your doctor | How tech can help you when isolated at home | How did this house survive an inferno? | The new bike you can ride on water | Fake news infects health and politics | Watchful eye on the metadata watchers
On social media Dr Phelps said there had been confusion about the initial rollout. “Our practices are meant to start with these items. To be frank, it is a very clumsy set of instructions.
“Many GPs I have been talking to are not clear what we can and cannot do under these arrangements especially in regard to bulk billing.”
Avoiding face-to-face consultations where possible has many benefits. Patients are spared from attending a GPs practice where they may fear being in contact with undiagnosed COVID-19 sufferers.
University of NSW virologist Professor Peter White said that if a doctor became ill at work with COVID-19, the whole practice may have to quarantine for 14 days. “If it’s a large surgery of 12 doctors, they’re all going to have to self quarantine and the doctor’s surgery will have to shut.”
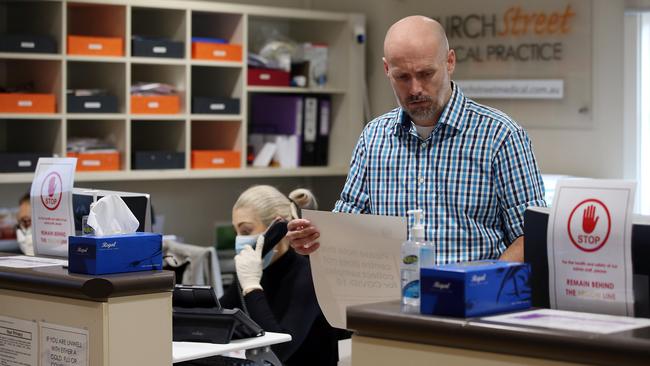
Suburban practices are making major adjustments to prevent infection in waiting rooms and surgeries.
Every 15 to 20 minutes, Newtown’s Church Street Medical Practice in Sydney’s inner west disinfects door handles and its payments’ terminal where patients punch in card details. Patients use every second chair when waiting, all magazines and toys have been removed, and payments are strictly cashless.
Practice manager Lachlan Stockbridge said he planned to isolate part of the surgery as a flu clinic and send patients there for shots to avoid contact with others. The practice was already offering phone and video consultations with Zoom.
A lot has to fall into place for telehealth consultations to work. Doctors and patients need computers, phones or tablets to talk with one another, and the internet has to work at both ends. If all else fails, there’s phone consultations.
Dr Phelps said doctors needed access to patient records when consulting from home. They’ll either need duplicate records at home, or have an ability to connect to their surgery’s computer system using remote access software.
Doctors and patients use video calling package that work for them. It could be a specialist telehealth package, or calling apps such as Zoom, Skype, Messenger Video and WhatsApps video.
Some practices are installing professional televideo systems. Anthony Fighera, of Melbourne-based CollabCare, said the company was installing more than 50 of its TeleConsult platforms.
Its platform provides video consultations and secure data management for clinicians. Patients click on a browser link to join video consultations.
Telehealth can make a big contribution to reducing face-to-face consultations in aged care.
Sachin Patel, founder of Aged Care GP, said his company provided care to 70 aged care health facilities in Melbourne. It had now been implementing telehealth. He said there had been no financial incentive to do this before March 13 when it became funded.
Health professionals either phoned or video called elderly patients who had smart phones, tablets and laptops. Patients were assisted by facility staff who by agreement took part in consultations when they centred on patient care.
Medication reviews, chronic disease management and care planning could be managed remotely. Telehealth also sped up the responsiveness of health professionals who didn’t commute as much between aged care centres.
Telehealth is not new, but until now patients bore the full cost of consultations. Brisbane’s Doctors on Demand has offered GP video consultations Australia-wide since 2016.
CEO Kirsty Garrett said demand had increased 300 per cent since February 20. “We are getting a lot of people who feel they have symptoms that look like COVIT-19 and they're looking for assurance, and also assessment to determine if they need to physically go to a bigger clinic, or need to have a test.”
She said Doctors on Demand had been reaching out for more GPs to address a shortage.
Some say telehealth has been an under-utilised service in Australia, and its wider implementation is long overdue.
Professor Anna Peeters, Professor of Epidemiology and Equity in Public Health at Deakin University, said that for Australians disadvantaged by distance or unable to easily leave the house, telehealth offered the chance to readily access health services by phone or video conferencing, particularly specialist health services that are hundreds or even thousands of kilometres away.
“While many recognised the opportunity offered by widespread telehealth availability, it has been held back by traditional financing, regulatory and delivery models, along with the lack of standard technology across our health system.
“That is now about to change. After opening up a Medicare item for selected telehealth consultations for those requiring COVID-19 isolation in early March, the government is now offering rebates on a much wider range of telehealth consultations.”



To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout