Healthcare must lift productivity or patients will pay more: Medibank boss David Koczkar’s plan to transform the sector
A failure to lift productivity will make access to healthcare more expensive, but Medibank boss David Koczkar has a plan to transform the sector.

A failure to lift productivity will make access to healthcare more expensive, with the sector lagging behind the national average, Medibank has warned.
Australia’s biggest private health fund has called for more partnerships between insurers, hospitals and governments to eliminate silos that have restricted innovation and created inefficiencies in the sector.
“We need to change the way healthcare is delivered in this country in order to sustain patient outcomes, increase affordability and access and ultimately improve productivity,” Medibank chief executive David Koczkar said.
“Investment in health innovation is the answer. By working together, insurers, providers, hospitals and governments can partner to deliver patient-centric services that increase accessibility to healthcare and take pressure off the health system.”
Mr Koczkar has joined other business leaders who have called for efforts to boost productivity. The recent federal budget raised concerns about sluggish productivity forecasts, forcing Treasury to cut long-term economic growth estimates.
Meanwhile, the Reserve Bank has become increasingly worried that flatlining productivity will make it harder to achieve inflation targets without higher rates.
However, healthcare is a very territorial sector in which insurers are seen as simply “the payers” and hospitals and clinicians “the care providers”, with little room to move in between.
While other funds, including NIB and Bupa, have also called for a more collaborative approach, they have largely been met with resistance from healthcare providers, which fear such a move will lead to US-style managed care.
McKinsey found Australia’s healthcare system had averaged annual productivity growth of 1.9 per cent in the seven years through to 2022, lagging other key industries. This is despite it recording the biggest increase in employment, with an annual growth rate of 4.8 per cent.
Agriculture and manufacturing both surpassed healthcare, recording productivity growth rates if 9.2 and 3.7 per cent respectively, while both sectors’ workforces shrank by 1 per cent.

Mr Koczkar said: “The opportunity for improved productivity in healthcare is clear as healthcare spending continues to grow, as does the burden of chronic disease and the ageing population.
“If the entire healthcare sector works together it can find a way to meet the growing demand for health in a sustainable way. While health innovation can boost productivity, it also improves access to quality healthcare.”
There have been a series of high-profile funding disputes between hospitals and health funds in the past year, with hospitals seeking to recover spiralling healthcare costs as their earnings were battered by elective surgery bans during the pandemic.
The sector is also battling a labour crisis, with Australia needing 85,000 workers by 2025, according to a federal government report published before the pandemic. Since the onset of Covid-19 the shortfall has worsened because of three years with no skilled migration.
The health insurance industry group, Private Healthcare Australia, has warned of double-digit premium increases if funds capitulate to hospital demands – as was the case when the feud between Australia’s biggest private hospital operator, Ramsay Health Care, and Bupa reached its zenith last year.
Meanwhile, almost four million Australians face higher private health insurance premiums in two weeks, after hikes were deferred during the pandemic.
Earlier this month, Ramsay Health Care chief executive Craig McNally said staff productivity had yet to rebound and was about 5 per cent below 2019 levels.
“We certainly as an industry haven’t done enough to address the work that wasn’t done over the last couple of years,” Mr McNally said.
“What we’re seeing – I don’t think this is necessarily a good or bad thing – but doctors practising that work/life balance is still there. Generally, doctors aren’t over-working to address that goal and operating at a comfortable level. We see that reflected in less after-hours work, less weekend work.”
Mr Koczkar said Australia also lagged behind other countries in adoption of new care models such as short hospital stay surgery and at-home care.
According to OECD data and LEK Executive Insights, international best practice – the US – is that 30 per cent of joint replacements are performed in short-stay hospitals, whereas in Australia it is close to zero.
The same data shows 90 per cent of hernia procedures are performed in short-stay hospitals – referencing The Netherlands as best international practice – but in Australia it is 24 per cent.
“A greater uptake of new care models will reduce the burden on a healthcare system already under pressure, freeing up capacity, and allowing future investment in more fit-for-purpose and less expensive settings,” Mr Koczkar said. “These changes are needed across the entire health system. Medibank is investing to bring new health programs to our customers which provide greater choice for patients in how their care is delivered and provides them with a better customer experience.”
While some hospital groups have resisted overtures from health funds, others have been more welcoming. Not-for-profit Catholic healthcare group Calvary has entered a joint venture with Medibank in South Australia to deliver SA Health’s My Home Hospital service, which involves providing hospital-type care within a patient’s home.
Mr Koczkar said the service had a complication rate “well below traditional bricks and mortar hospitals” while generating a patient satisfaction score of 96 per cent.
“We are also doing this through the North Coast Health Connect service we deliver on behalf of the NSW government – which is a free 24/7 registered nurse service for all Northern NSW residents – aiming to improve access to local healthcare.”
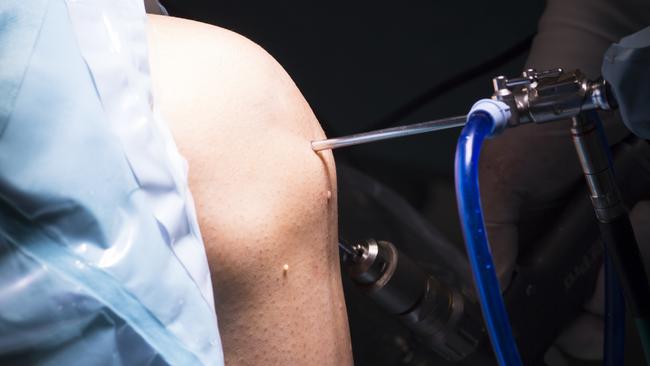
It has also struck partnerships with Healthe and Aurora Healthcare. “Our partnership with Healthe Care is saving people thousands of dollars in out-of-pocket costs for short-stay knee or hip replacements and helping relieve pressure on the stretched hospital system,” he said.
Our partnership with Aurora Healthcare, to boost access to mental health care and support including in-home care, is another investment in health innovation we are making.
“In doing this we are helping change our health system, so it is sustainable for the generations to come.”







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout