One in nine women have a health condition costing $30,000 a year
It's a health condition that has been shrouded in shame and dismissed by medicos for hundreds of years, and major changes to the health system are needed to give sufferers a fair go.
Health
Don't miss out on the headlines from Health. Followed categories will be added to My News.
One in nine Australian women suffer from crippling pelvic pain that is often dismissed by doctors and costs them up to $30,000 a year in health costs and lost income.
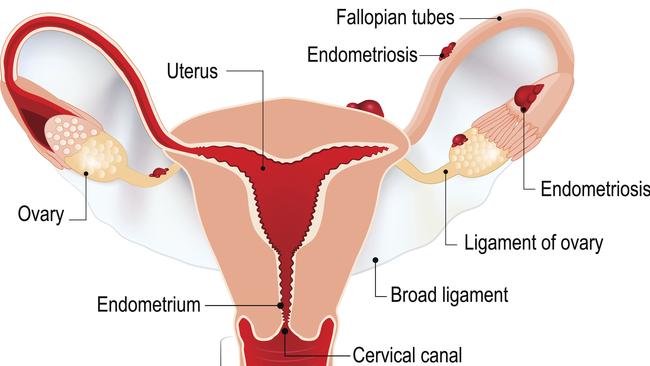
Close to one million women have endometriosis – a painful inflammatory disease where tissue similar to the lining of the uterus grows in the pelvis, the bowel and other organs.
A News Corp investigation has found despite a national action plan for the condition put in place five years ago, women are waiting more than six years for a diagnosis.
One woman we spoke to went to 14 doctors over five years, with all of them dismissing her symptoms, including one she claims laughed at her connecting regular vomiting and diarrhoea symptoms to her periods.
When sufferers eventually do get referred to a specialist, most face a wait time of around six months for an appointment, and another 18 months to three years for surgery in a public hospital.

While there is a new Medicare rebate for an MRI for endometriosis, a free specialist ultrasound to diagnose the condition has a wait time of between three and six months in the public system, while a privately funded scan costs $500 with a Medicare rebate of just $83.
Private Healthcare Australia data shows privately insured women face typical gap fees of $1715 for a hysterectomy, while others paid gaps of $4200.
Gap fees for complex laparoscopies – a procedure where a tiny camera is inserted into the abdomen to diagnose and treat the condition – typically cost $1250 according to Private Healthcare Australia. But some women are paying as much as $4000.
“It’s usually about $4000 out of pocket with full top table private health insurance, to have laparoscopic surgery, and that’s got to be done regularly,” Endometriosis Australia chief executive Maree Davenport said.

“Just even going to a GP, they’re out of pocket, usually … $60 to $70,” she said.
One in 13 women self-fund their private procedures with out-of-pocket costs of $10,800 for a hysterectomy and more than $8100 for a laparoscopic resection of endometriosis to treat severe disease.
Many women require up to 10 laparoscopies over a number of years to treat the condition that often recurs after surgery.
A survey of more 400 women with the condition found they were spending on average $480 every two months of their own money to cover expenses for physiotherapy, massage, naturopaths, acupuncture, dietitians and pain therapies.
The drug Visanne, developed specifically for treating the condition, is not subsidised and can cost between $70 and $110 per month.
“Endometriosis is a very expensive disease to have,” University Western Sydney reproductive health expert Professor Mike Armour, who has conducted multiple studies into the financial burden of the condition, said.
“We know that endometriosis costs on average around $30,000 Australian dollars per person per year, that’s a mixture of out of pocket and societal costs,” Prof Armour said.
“You’ve got a group of people who are often financially struggling because they’re unable to work full time. And then on top of that if you want to manage your symptoms you’re going to have to find considerable money out of your own pocket.”
Ernst and Young calculated the condition costs the health system more than $500 million a year, with a further $2.6 billion a year in productivity losses as a result of time off work.
Over a woman’s lifetime, the condition could cost her $129,000 in reduced quality of life.
Professor Armour said there was a major gender imbalance in Medicare where rebates for ultrasounds of men’s private parts attract higher rebates than those for women’s.
Roughly the same number of people have endometriosis as have diabetes and heart disease yet endometriosis receives a fraction the funding these diseases received, he said.
The health system spends almost $12 billion on cardiovascular disease and over $3 billion on diabetes each year, but just $500 million on endometriosis.

Federal Assistant Health Minister in charge of women’s health Ged Kearney said “too many women suffer for years with what we know can be debilitating conditions. They deserve to have their concerns be taken seriously with better access to specialised care”.
The government has set up a National Women’s Health Advisory Council and introduced a Medicare rebate for a new 60 minute consultation in the May budget that “will particularly benefit women who often need more time with their GP to address complex health conditions such as endometriosi”, she said.
PREGNANT PAUSE TO THE SUFFERING
Kylie Brown had been dating her now husband Brisbane Lions’ star Jonathon Brown for just three months when her painful heavy periods were diagnosed as endometriosis.
Her doctor had found an endometrioma – a cystic lesion the size of a golf ball above her pubic bone. The tissue was also growing on her bowel and bladder.

Jonathon was in the consultation when the doctor told her “the best thing is to start trying for kids sooner rather than later”.
“And I remember not being able to get eye contact with my new boyfriend,” Kylie said. “Luckily he stuck with me.”
The couple did what the doctor ordered and Kylie endured six pregnancies including two miscarriages and an ectopic pregnancy to give birth to three children: Olivia, 13, Jack, 10, and Macy, 8.

“The pregnancies were probably the most pain free time because of the hormones and everything actually does slow down the growth,” Kylie said.
She has had a hysterectomy to try to relieve her pain and tries to not talk about it because “it’s such a boring conversation because no one can help with the pain.”
A key strategy is to set herself goals, such as running a marathon, which she managed nine months after her ninth surgery and raised $27,000 for Endometriosis Australia in the process.
‘I CAN’T KEEP LIVING WITH THIS PAIN’
Paralympian Monique Murphy dearly wants children but will have a hysterectomy next month because “I can’t keep living with this pain”.
The 29-year-old Paralympian suffers from a double whammy of pelvic pain caused by adenomyosis where tissue grows into the muscle of the uterus wall as well as endometriosis where the tissue grows outside the uterus.
Her symptoms include blistering in the uterus, extreme fatigue, pelvic pain and Inflammatory Bowel Syndrome IBS symptoms.

A spiked drink caused her to fall off a balcony when she was 19 and her leg was amputated below the knee but she said her endometriosis has had a greater toll on her sporting performance than the injuries from the fall.
“I haven’t raced that perfect race. I haven’t given it my all and have the sense of not knowing what I’m truly capable of because I’ve been hindered by this condition,” she said.
She saw 14 doctors in five years before she was finally diagnosed and learned more online from other sufferers than from the medical profession.
Together with surgeries to repair her body after her fall she has had 27 procedures and she says the out of pocket expenses for endometriosis are almost double those for non- gender based surgery.

A two week stay in hospital for major knee and ankle surgery left her $3,000 out of pocket but the hysterectomy will cost her $5,000.
“From my experience it seems to be you incorporate the uterus and the price goes up,” she said.
She has spent tens of thousands of dollars on endometriosis treatments.
“It’s where all my paycheck goes. We don’t get much being an athlete but it’s where every last bit of money has gone along with support from parents. It’s very financially consuming.”
Despite having top private health cover she is $170 out of pocket when she sees a pelvic physiotherapist and $80 out of pocket for a regular physiotherapist.
“There needs to be financial support in getting the surgery and managing the condition and looking at the condition from a holistic point of view,” she said.
WHAT NEEDS TO BE DONE
b Establish a centre of excellence endometriosis clinics in a major public hospital in each state.
b Allow telehealth consults with these clinics for patients in rural and regional areas.
b Raise Medicare rebates for laparoscopies, hysterectomies, doctor consults and ultrasounds.
b A new Medicare rebate for pain education by medical, nursing or allied health practitioners.
b Fund extra public surgeries to end the three-year wait for laparoscopies and hysterectomies.
b Double the number of allied health visits funded under a chronic disease plan.
b End the six-year diagnostic delay.
b Extend the Pelvic Pain Education Program (PPEP) talk on pelvic pain to all schools.
b Collect better Medicare data on the condition and spend more money on research.
b Fund Endometriosis Australia to provide training to GPs and nurses.
DEBILITATING CONDITION DOCTORS WON’T TREAT
Before modern surgical techniques allowed doctors to see the endometrial lesions causing women severe pain, sufferers were dismissed as ”being hysterical”.
There was no research into its causes, and even today treatments are under researched, very basic and often ineffective.
“Women’s pain has not been taken seriously. Women are constructed as being hysterical, overreacting, the pain is in their head. And, unfortunately, this is something which has been quite slow to change,” University Western Sydney reproductive expert Professor Mike Armour said.
“Many people with endometriosis have mental health issues, not only from the chronic pain, but also the medical dismissal and gaslighting,” he said.
In 2018, then Health Minister Greg Hunt formally apologised to women that nothing had been done sooner when he announced the first national action plan for the condition.
But five years after it was launched, women with the condition are still plagued by delayed diagnosis, and delayed access to treatment and spiralling medical costs.


We’ve spoken to experts and patients around the country about what more needs to be done to help women get a faster diagnosis and a quicker end to their pain.
“GPs self-report that they don’t know enough about pelvic pain, and it’s not taught in a lot of universities and, if it is, it’s one hour, that’s all they get.,” Pelvic Pain Foundation executive director Kirsty Mead said.
“So you go to the local doctor, the doctor says ‘well, suck it up’, that’s how it is,” Ms Mead said.
To overcome this lack of medical training, the Australian Coalition for Endometriosis has called for specialist endometriosis clinics to be funded in major hospitals.
They would be staffed with experts in the condition and would be centres of excellence that could provide expert care particularly for those in the bush.
“Every state should have one and they should have telehealth capacity because women don’t need to be travelling,” Ms Mead said.
A new Medicare rebate is also needed to cover the long appointments needed to diagnose the condition experts and patients told us.


Gynaecologists Professors Luk Rombauts and George Condous said a recent international conference heard, while there was a place for surgery, more treatment should focus on managing pain.
There is a $420 gap payment for a special ultrasound to diagnose endometriosis so the rebate needs to be increased to help patients with the cost and provide an incentive for more clinics to train people to carry out the scan, Professor Condous said.
Medicare rebates for hysterectomies and laparoscopies also need to be raised to ease the massive gap fees in private hospitals.
People with a chronic disease should be able to access a chronic disease management plan to pay for five allied health sessions, but only 15 per cent of women with the condition have one.
Prof. Armour said the number of sessions it covered needed to be increased because women needed ongoing access to care.

The Albanese Government has given 20 GP clinics $700,000 each to provide expert care and they are due to open later this year. But doctors working in them have told News Corp they will bill patients for treatment – something which needs to be reconsidered.
And Endometriosis Australia CEO Maree Davenport said the doctors at these clinics were asking her charity for education resources and training on the condition even though they get no government funding.
The government’s national action plan wants awareness about endometriosis raised but the Pelvic Pain Foundation’s school-based education campaign is funded in only 20 per cent of schools, which the Foundation believes should be expanded to every school.
There also needs to be a new Medicare rebate for nurses and allied health practitioners to provide pain education to sufferers, like the rebates available for diabetes education.
World leading Australian research is working on finding better ways to diagnose and treat the condition but more funding is needed.

The University of Melbourne’s Professor Peter Rogers and Perth-based company Proteomics International are developing a new blood test to diagnose endometriosis and using a bank of donated endometrium tissue to determine which types are more severe.
Prof. Rogers is also testing whether a food supplement, Palmitoylethanolamide (PEA), might ease the pain.
University of Adelaide researcher Louise Hull is using artificial intelligence to refine ultrasounds and MRI scans to develop non-invasive scans for the condition.
A Monash University study led by Dr Jane Varney is testing whether a diet change can help control the inflammatory symptoms of the condition.
Prof. Armour is trialling the use of medicinal cannabis to relieve the pain.
Research published last week found two -thirds of women with endometriosis had a bacteria called fusobacterium in the lining of their uterus which could provide a target for new treatments.
Ms Davenport said the condition was slowly being recognised and the stigma was easing but doctors and the community needed to realise “those one in nine women, almost all of them have it that severely that it absolutely defines their lives”.
More Coverage
Originally published as One in nine women have a health condition costing $30,000 a year





