Decline in mental health care in NSW hospitals during pandemic
A bombshell report has shone light on Australia’s treatment of hospitalised mental health patients during the pandemic, and it’s not good.

A new report has found mental health patients in NSW hospitals are suffering under worse care conditions during the coronavirus pandemic, as they’re subjected to more severe, non therapeutic interventions.
There was a rise in the number of times mental health patients were secluded or physically restrained while in mental health treatment, according to the Healthcare Quality Trend report on NSW hospital performance from April to June 2020.
According to the report, these interventions are detrimental to a patient’s health, and should only be used as a “last resort”.
Mental health patients have also been subjected to longer periods of seclusion since the coronavirus pandemic.
Seclusion periods peaked in the January to March period at an average of nine hours and 45 minutes. In the April to June period, seclusion events lasted for an average of seven hours and 16 minutes.
The report describes seclusion as “when a patient is placed alone in a room or an area at any time of day or night, with no freedom of exit”.
“Such restrictive intervention is not therapeutic and should only be used as a last resort when other options have been unsuccessful in maintaining safety for the patient, staff or others.”
“There is a high degree of variability quarter on quarter, but the trend has been rising in recent quarters,” the report said.
The report did note since 2016 the overall number of seclusion events had fallen from 1159 in April to June 2016 to 866 in April to June 2020, down 25.3 per cent.
RELATED: Victoria’s top cop notices worrying lockdown trend
RELATED: 15 minute test to predict disorder
The NSW Health Performance previously set a target, or KPI, in 2017-2018 for the duration of seclusion, that a patient wouldn’t stay isolated for more than four hours. However, the report noted that the average period of seclusion has “been longer than four hours since July to September 2017”.
RISE IN PHYSICAL RESTRAINTS
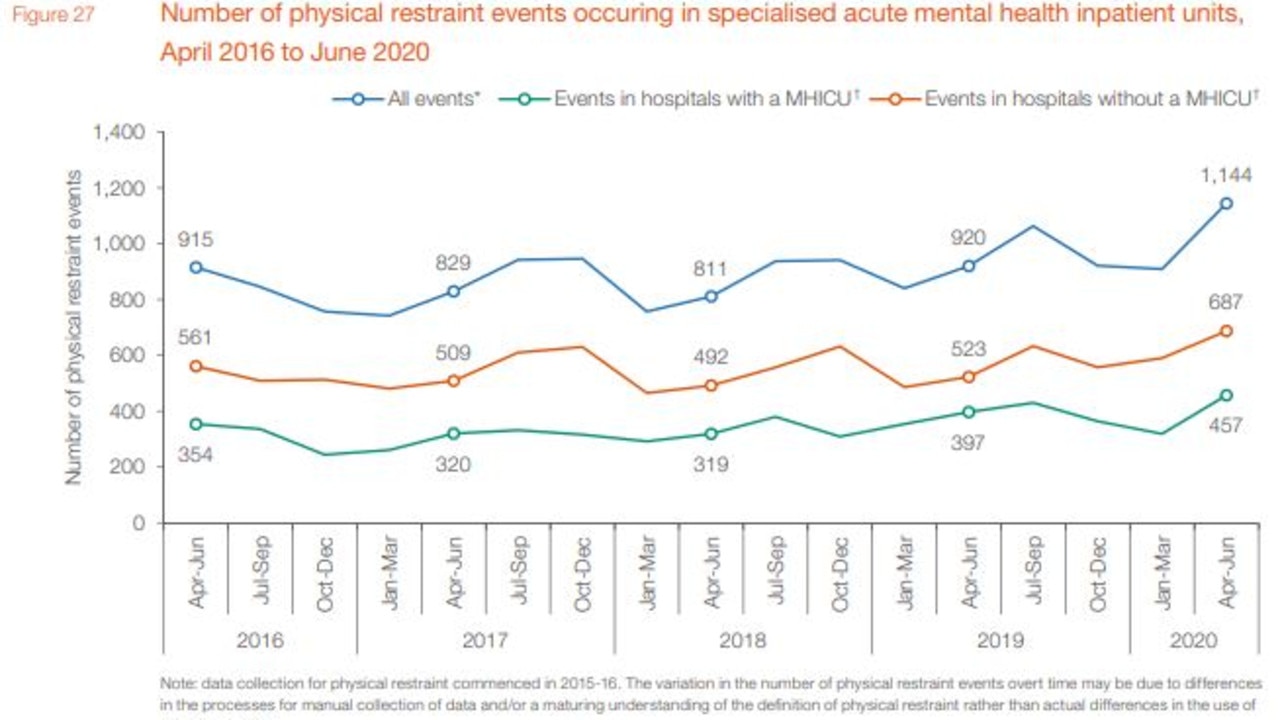
The number of times patients had been physically restrained had also risen 25 per cent since 2016.
The total number of physical restraint events has risen from 915 in April to June in 2016 to 1144 in the same period in 2020 — the report noted there had been some seasonal variation in the interim, before a recent rise.
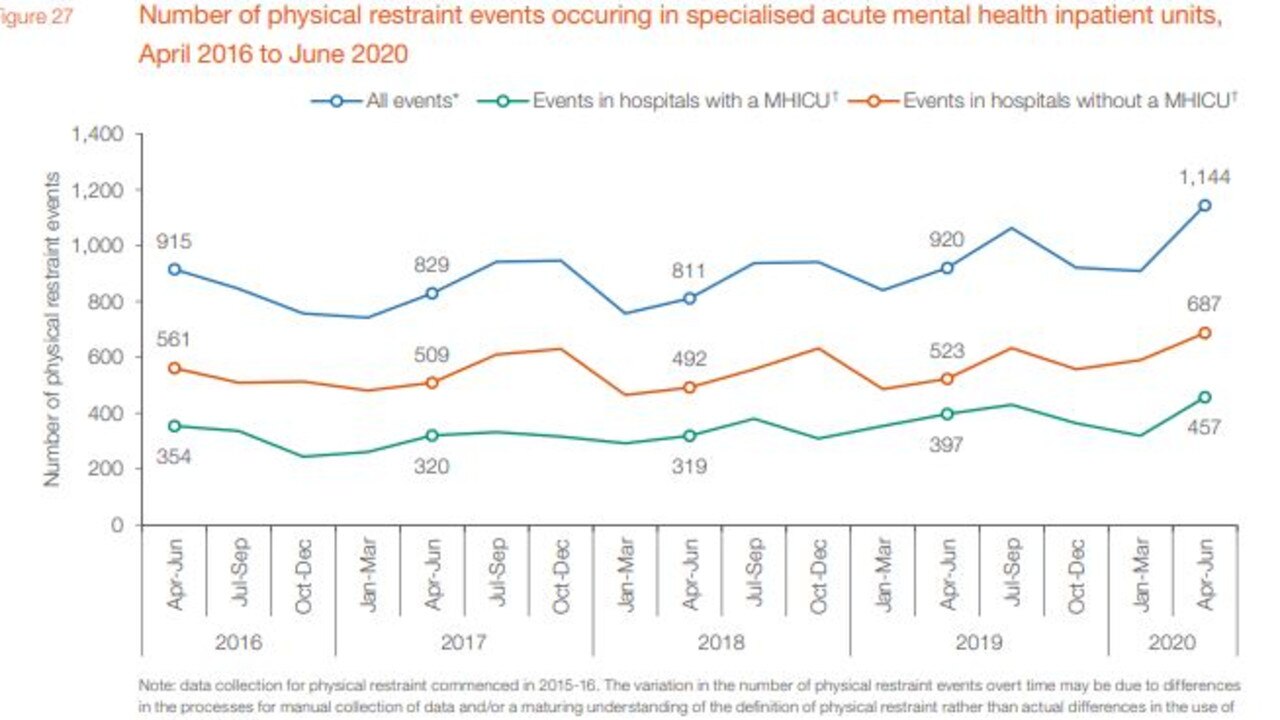
Physical restraint in a mental health setting occurs when the “patient’s freedom of movement is restricted by physical means (i.e. the hands-on immobilisation by health care staff),” the report read.
Similarly to seclusion, physical restraints are described as being “not therapeutic and should only be used as a last resort when other options have been unsuccessful in maintaining safety for the patient, staff or others.”
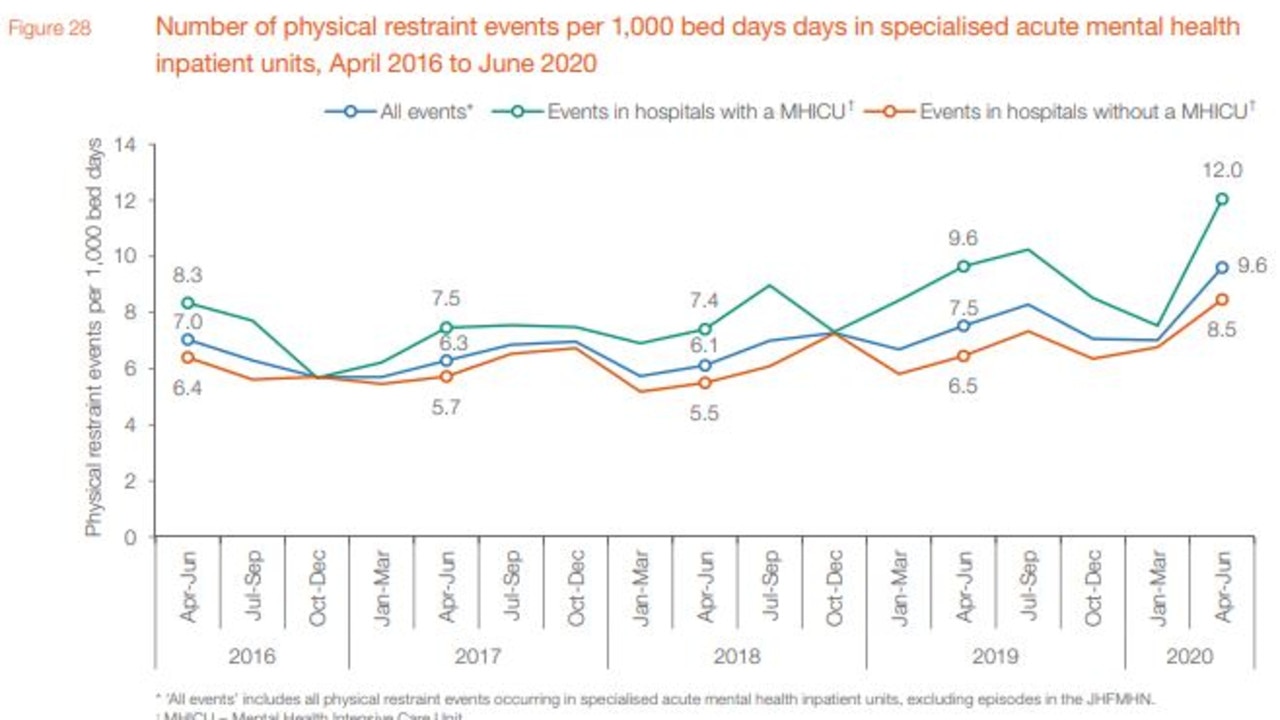
The average time a patient was physically restrained has varied, although is typically longer in a hospital with a mental health intensive care unit than one without.
The report noted the majority of episodes in acute mental health care wards at NSW public hospitals don’t involve any form of physical restraint.
In the April to June period this represented 94.7 per cent of acute cases, which had no physical restraint.




