Pink Army backs breast cancer breakthroughs
EACH generous dollar raised from tomorrow’s Mother’s Day Classic, goes straight to the scientists who have the skills to find the cures, and to develop smarter treatments for breast cancer.

VIC News
Don't miss out on the headlines from VIC News. Followed categories will be added to My News.
IN hues of fairy floss, neon candy and watermelon, and some wearing fairy wings, tutus or outrageous wigs, they will lace up their runners tomorrow in their thousands.
But don’t be fooled by the brightness and frivolity. They will be out in force against one serious foe.
Breast cancer steals mothers, daughters and girlfriends too soon. It robs wives, sisters, aunties, grandmothers and work colleagues of life.
Tomorrow, at parks across the country, including Melbourne’s Royal Botanic Gardens and 31 sites in country Victoria, thousands will don the pink uniform to run or walk in the Mother’s Day Classic.
More than 1.2 million Australians have taken part in the event over the past 21 years, helping raise more than $33.2 million for breast cancer research through the National Breast Cancer Foundation.
Each step is a collective one towards a world with zero breast cancer deaths. Each generous dollar raised — from teams pooled in memory of friends taken too soon, or as a morale boost to those undergoing treatment — goes straight to fund scientific research.
These scientists have the skills to find cures, and to develop the combination treatments that seek and destroy cancer cells in smarter ways while dodging side effects.
Here are three research projects that will be funded this year through the efforts of those taking part in tomorrow’s charity event:
ALL women would have an initial mammogram around age 30 to reveal the density of their breasts, a screening that would reveal their lifetime cancer risk.
That’s the grand aim of Professor John Hopper, a University of Melbourne statistician who is making significant inroads into revolutionising breast cancer detection away from mass screening to personalised prevention by better identifying women at high risk.
His breakthrough work, published two years ago, found that looking at white or “bright” areas of breast density on a mammogram, rather than duller areas, is 30 per cent more accurate at predicting future cancer risk. It is even more reliable than assessing genetic markers.
“Current screening starts at 50, but a lot of women have got nasty breast cancers by then,” Hopper says. “If we screened women at around 30, and then if it looks like they’re at risk, they would have genetic testing to pick up high-risk women at a younger age. Women at low risk could come back at age 50.”

His NBCF funding of almost $500,000 over the next three years will allow him and his collaborators to train radiologists across the country to interpret these new risk score measurements in standard and newer digital mammograms. It is an important step on the road to making this risk assessment standard care.
The team is also starting a prospective study of about 25,000 women who have had a digital mammogram over the past five years, taking data from two Breast Screen Victoria studies, to see how accurate the new risk assessment technique is at detecting cancer risk.
“By combing these new measures based on the mammogram with family history data and genetic markers, we can identify 10,000 more women a year who are at risk than if we looked at who has a genetic mutation,” Hopper says.
EXCITING new immunotherapy treatments that re-engineer the body’s immune system to recognise and seek out cancer cells are among the newest and most promising cancer treatments.
And while CAR T-cell therapies, only available in Australia on a sparse number of clinical trials, are keeping many blood cancer patients in remission, these engineered immune cells are not yielding the same results in solid tumours such as breast cancer.
But Dr Clare Slaney, a senior researcher at the Peter MacCallum Cancer Centre, is working to overcome this stumbling block by developing a new type of molecule to be given alongside an injection of CAR T-cells, to boost its effectiveness.
“It’s really difficult for CAR T-cells to find the location of the cancer in solid tumours,” Slaney says. “Even if they do, they don’t proliferate. Solid cancers also usually have an immunosuppressive tumour marker on their surface, so they don’t react to fight the cancer.
“We need to find a way to make CAR T-cells find the tumour, and then expand a lot to give out the trafficking information to rally other cells to come and fight the cancer.”
Not only have Slaney and her team been able to eradicate breast cancers — and the metastasis — in mice using this combination treatment, but it has also protected the animals against the cancer returning.
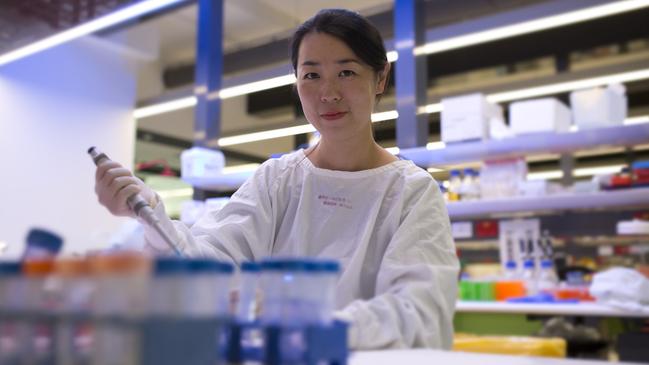
Slaney has this year been awarded the Mavis Robertson scholarship, which recognises the brightest female researchers who also show leadership abilities. This NBCF funding will allow her to hire a research assistant so they can complete further animal studies using a molecule that would be more applicable for use in humans.
She also plans to use the money to learn a type of computer programming she hopes can help her extract secrets from human tumour samples to boost her immunotherapy combination.
CHEMOTHERAPY has been a vital tool in the armoury against cancer for more than 50 years. But its side effects can be severe.
Not only does it cause hair loss, fatigue, nausea and infection, but from the first dose of the common chemo drug doxorubicin, it causes cumulative heart damage.
But Dr Suzanne Cutts, from the La Trobe Institute for Molecular Science, is developing a way to boost the effectiveness of chemotherapy at treating cancer that has spread, while also protecting the heart.
“It gets to a point where women can no longer receive the chemotherapy any more because of the heart damage, even if it’s effective at treating their cancer,” Cutts says.
“If we could make traditional therapies better by just doing one thing to it, not changing what they’re getting but adding something, that would make it that much better.”

Her research team has used doxorubicin in combination with a “prodrug” that releases formaldehyde, a medicine that only becomes active once released in the body.
Cutts says while this chemical is most well-known for preserving dead bodies, it has emerged as a crucial ingredient in the process of inhibiting the growth of cancer cells. Her research with her Israeli collaborators has revealed that a combination of this formaldehyde-releasing drug alongside chemotherapy protects heart cells in animals.
After missing out on funding for this project from the National Health and Medical Research Council three years running — a funding source where only about 15 per cent of applications are successful — Cutts says funding opportunities such as the NBCF are crucial to meaningful medical research discoveries.
Her funding this year will allow researchers to further test the combination in animal models using medication already on the market, to look at their effect on metastases.
They are also developing “nanoparticles”, in which the prodrug will be encased so it can be protected and not break down until it reaches the site of the tumour.
MOTHER’S DAY CLASSIC ENTRIES ARE STILL AVAILABLE AT THE EVENT TOMORROW (SUNDAY, MAY 13).


