New national study reassures infertile men that ART works
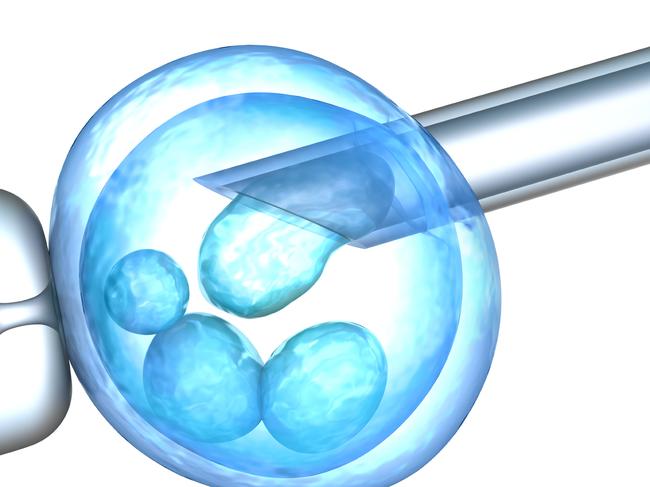
A landmark Australian study on 36,000 couples offers reassurance to infertile men that modern IVF can work just the same for them as it does fertile men.

Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Modern IVF has levelled the playing field for men experiencing infertility, a landmark Australian study shows.
For the first time it offers reassurance to infertile men that if they have assisted reproductive technology (ART) with their partners they can expect similar pregnancy outcomes to fertile men having the same treatment.
“It is good news for couples,” Professor Robert McLachlan said. “But this is just the first step, there’s a lot more research on male infertility to be done.”
The results of the study were presented at the Fertility Society of Australia and New Zealand (FSANZ) conference in Perth on Monday.
They are the outcome of a study by the University of NSW’s National Perinatal Epidemiology and Statistic Unit looking at male infertility and its impact on ART.
The study involved more than 36,000 couples using information collected through the Australian and New Zealand Assisted Reproduction Database (ANZARD).
This unique registry collects information on all ART treatment cycles in Australia and New Zealand.
Prof McLachlan, from the Hudson Institute of Medical Research, Monash University and a consultant with Monash IVF, is a male reproductive health scientist who was involved in the study.
“We found that whether you have in your history damaged sperm production from cancer treatment or from some traumatic event or infection or even genetic anomalies, providing the sperm can be isolated, they perform and produce similar (pregnancy) outcomes,” Prof McLachlan said.

“The message is that it’s very reassuring that there’s a level playing field for couples with all types of male infertility.”
Infertility is defined as the inability to conceive after a year of unprotected sex, or unable to carry a pregnancy to a live birth. It affects about one in six couples and 40 per cent is related to male factor infertility.
Prof McLachlan said Australia was the only country with a large database that now also collected the causes of male infertility.
“Until this change we had one diagnostic category entitled male infertility,” he said. “The reality is that there are multiple causes and degrees of severity in male infertility, and it had been unclear how specific causes impacted the chance of successful ART treatment.”

Prof McLachlan is also the medical director of Healthy Male, the free website funded by the federal government to provide education in male reproductive health.
“This (study) is the beginning of the road,” he said.
“I’d like to see a time where we can really tell people which particular type of male infertility is the cause because now when I am asked why, sadly I often have to say I don’t know why a man’s sperm production is poor because the precise cause is unknown.
“But happily this study shows if we can get even a single sperm we can often resolve the problem.”
Prof McLachlan said the annual ANZARD report released on Friday was a positive for the IVF industry.
“It demonstrates that it is possible to collect meaningful data from all 100 or so centres around Australia, put them together, and then analyse them to the benefit of the patients and the doctors for counselling,” he said.

AT A GLANCE
The annual ANZARD reported:
•More than 20,000 babies were born through IVF
•Around 108,000 ART cycles were carried out, one in three because of male infertility
•The average age of women turning to ART was 36 years, one third were single women or female/female couples
•Most male infertility is unexplained
•Frozen cycles (31.8 per cent) had higher live birthrates than fresh cycles (14.7 per cent)
•One third of women achieved a live birth in their first complete ART cycle




