Neale Daniher’s FightMND delivers seven new research projects
You’ve made donations and bought the beanies, but what exactly is the money from the Queen’s Birthday fundraiser going to? Neale Daniher and the FightMND team have announced a raft of new projects funded by the $7.6 million raised from last year’s MCG Big Freeze.
VIC News
Don't miss out on the headlines from VIC News. Followed categories will be added to My News.
When Neale Daniher was diagnosed with motor neurone disease almost six years ago, there was not even a promising treatment on the horizon.
“When there is no drug trial, there is no hope. But now there is hope,” the AFL great said.
Today his FightMND foundation is announcing the seven new medical research projects to be funded by $7.6 million raised from last year’s MCG Big Freeze.
Three clinical trials, including a first-in-human study, will test promising therapies in humans.
Two new drugs, one of which involves an innovative way of sneaking in promising treatments across the impenetrable blood-brain-barrier, will be supported.
NEW DRUG SIGNIFICANTLY SLOWS MND IN ‘HUGE BREAKTHROUGH’
NEALE READY TO PASS THE FIGHTMND BATON
HONOUR REFLECTS ODD COUPLE’S UNIQUE BOND
There is also an ambitious plan to categorise different types of MND patients based on their genetic and molecular disease profile, to better predict who could benefit from what new drug.
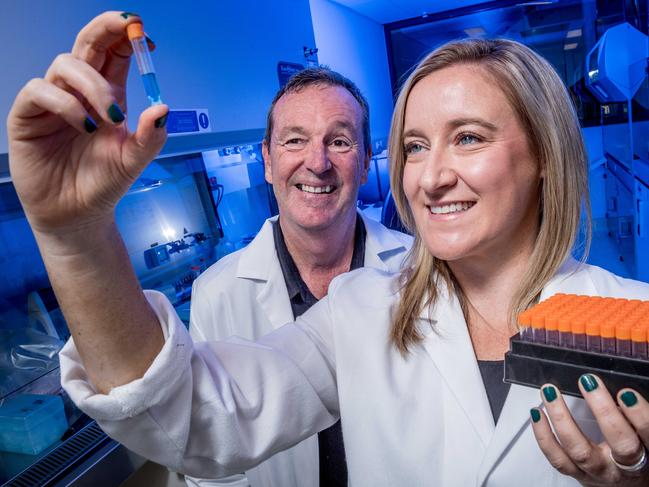
FightMND research manager Bec Sheean said it was a stringent review process to assess the 30 applications received researchers around the world.
“We look for evidence that a drug is likely to work; that it’s shown promise in animals, cell models, or in a similar disease,” Dr Sheean said.
“We look at if they are a research team with the expertise to deliver what they say they’re going to, and that the treatment they’re developing will be relevant to people.
“We have to keep advancing new drugs through the clinical trial pipeline until we find one that works.”
The funding pool includes $2 million of Federal Government funding, which matched dollar-for-dollar what was raised by the Australian public.
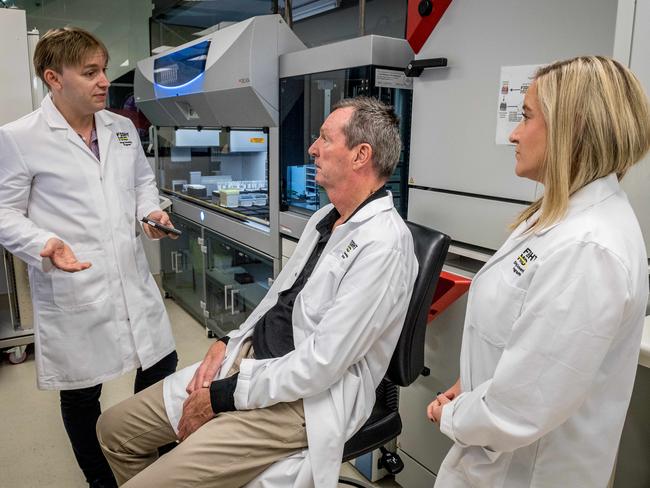
One of the key projects, the Precision Medicine Program led by Associate Professor Brad Turner at the Florey Institute of Neuroscience and Mental Health, will differentiate patients into disease subtypes.
The skin biopsies of 151 Australian MND patients — of which Daniher was the first to donate — have been turned into stem cells. Next they will become spinal motor neurons.
Using the $1 million custom-built robot the Florey received last year from FightMND, these human motor neuron cells will be tested with thousands of FDA approved drugs — everything from cold sore cream and aspirin, to antidepressants and blood pressure medication — to see if any medication already on the market can protect or repair human motor neuron cells.

And now, with their $2 million in new funding, Dr Turner and his team will drill down into the biological make-up of each individual’s disease to develop a “disease signature”.
“I think the reason MND clinical trials have failed in the last 25 years is we group all patients together, so you can’t detect the benefit,” Dr Turner said.
“But once we get a disease signature we can start to address the treatment according to that profile, so every patient benefits, just like in cancer That’s the key difference.”
But Daniher said the job was not done, and urged the public to continue supporting the cause.
“Don’t give up on us now,” he said. “MND is a beast. It’s a riddle and it will take some time to solve, but I’m hopeful we’ll find a treatment within five years.”
PROJECTS TO BE FUNDED BY FIGHTMND
CLINICAL TRIALS
1 The drug edaravone, which uses its antioxidant properties to protect nerve cells, is already approved for use intravenously in Japan and South Korea under the name Radicut.
Now, about 60 Australians will be among 300 patients recruited worldwide to the phase III trial, which will pit an oral version of the drug against placebo.
2 A small phase I safety trial of the Melbourne-designed drug copper-ATSM, also found in addition to being well tolerated that the capsule was able to slow the progression of the disease by 70 per cent after six months of treatment.
Now the phase II trial will test its effectiveness in 80 patients — half from Australia — starting in the middle of the year, through Calvary Healthcare Bethlehem in Melbourne and Macquarie University in Sydney.
3 Queensland Brain Institute researchers have designed a drug called mEphA4, which prevents the motor neuron death in mice with MND, increasing lifespan and improving function.
Now, a first-in-human trial aims to establish the drug’s safety, with the hope of seeing early signs of promise to inform a larger trial.

DRUG DEVELOPMENT
4 A new drug delivery system is showing promise at allowing important molecules to hitch a ride through the blood-brain-barrier and act directly in the brain and spinal cord.
Researchers from New York biotechnology company Lauren Sciences will now test whether this V-smart nanomedicine technology can reverse or slow progression of MND in mice, with the results to inform the phase I human clinical trial.
5 The University of Queensland will test a promising drug in mice called GRT-X, which has been shown in preclinical models to slow disease progression by “calming down” hyper-excitable motor neurons to protect them from damage.
The results will determine whether this is a suitable drug for human patients.
PRECISION MEDICINE
6 The Florey Institute of Neuroscience and Mental Health is leading a $2 million national program to uncover the unique genetic and molecular signature of each MND patient.
By recognising that MND is a heterogeneous disease, they are working to find the right drug for the right patient at the right time.
By differentiating patients according to their individual disease profile, they can better allocate patients to promising clinical trials.
7 South Australia’s Flinders University researchers have developed a urine test to accurately measure MND disease progression.
A new robotic system will test these patient samples to more accurately gauge whether experimental treatments in clinical trials is working or not, to direct promising treatments more quickly to the right patients.


