Melbourne scientists behind world-first cancer drug breakthrough
MELBOURNE scientists are developing a world-first drug that can control the immune system, potentially paving the way for thousands of cancer patients to have lifesaving immunotherapy.

VIC News
Don't miss out on the headlines from VIC News. Followed categories will be added to My News.
MELBOURNE scientists are developing a world-first drug capable of controlling the human immune system and potentially paving the way for thousands of cancer patients to undergo lifesaving immunotherapy.
The Peter MacCallum Cancer Centre team is fine tuning the drug which is able to temporarily suspend a person’s immune system to stop it attacking non-cancerous parts of a patient’s body or rejecting bone marrow transplants.
They hope to treat the first patients with the breakthrough perforin-inhibitor within the next two years under a clinical trial to determine if it can overcome dangerous side effects that currently leave about one in 10 patients unable to tolerate the latest cancer treatments, which act by activating the patient’s immune system to fight their cancer.
If successful, the process will hand doctors greater control of the human immune system to fight various forms of cancer as well as diseases such as malaria and diabetes.
Peter Mac’s executive director of cancer research Prof Joe Trapani believes the breakthrough will allow doctors to regulate a patient’s immune response so it can be focused solely on killing cancer.

“It’s no good being able to control a patient’s cancer but then causing life-threatening side effects too,” Prof Trapani said.
“About 10 per cent of patients treated with new immune-based therapies end up activating the immune system to the point where normal tissues are also in danger.
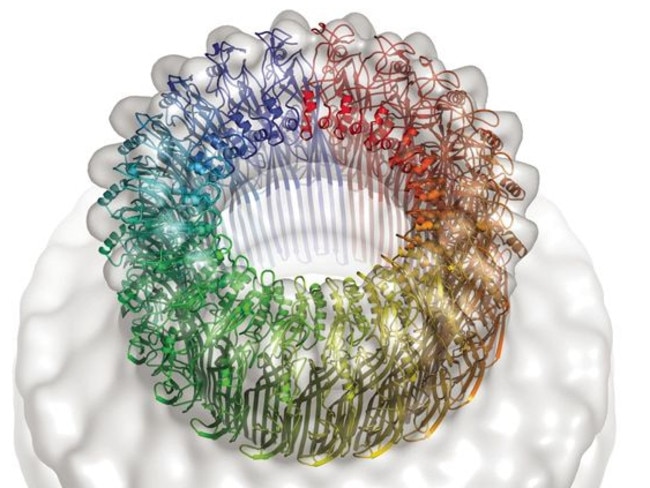
“There is the potential to intervene in various ways, and blocking perforin — a critically important bullet fired by the immune system against target cells — would effectively be putting up a temporary shield against those bullets.”
Immunotherapy breakthroughs in recent years have allowed doctors to switch on and supercharge a patient’s own immune systems so that it will overcome their cancer.
But in about 10 per cent of cases the beefed-up immune response also attacks a patient’s vital systems including their bowels, lungs and even skin, with life-threatening complications in some.
The new class of drugs developed by Peter Mac works to block a protein called perforin — which when activated punches holes in the surface of cancer cells to allow toxins to enter and destroy the disease — effectively suppressing a person’s immune system for up to a few weeks.
The culmination of 20-years research, the drug could also be used to stop a body rejecting foreign tissues such as bone marrow transplants needed to fight leukaemia.
The Melbourne research is of such international significance that it was one of the first non-UK projects ever funded by the Wellcome Trust, receiving $12.5 million over the past five years.
With clinical trials around the world opening up the chance to treat cancers including melanoma, lung cancer, colon cancer, breast, pancreatic and lung tumours, leukaemia, myeloma and lymphomas with “checkpoint” immunotherapy drugs, it is hoped the perforin-inhibitor will greatly expand the number of patients who can benefit.
Wonder’ cancer drug saves mum’s life
KRISTEN Pickford was having scans every few months for five years to make sure her cancer hadn’t returned.
But on her last scan doctors learned the worst.
The mother-of-two had a cancerous spot on her liver and she’d need lifesaving surgery.

“I wouldn’t be here now if I didn’t have those scans. We are so lucky I was having them,” she said.
Five years earlier, Ms Pickford was diagnosed with melanoma while pregnant with her second child Harley.
She had the cancerous spot taken from her neck, but three months later, the cancer spread and she needed 28 lymph nodes removed.
When a new clinical trial at Peter MacCallum Cancer Centre opened — involving several injections and scans every six weeks for five years to ensure the cancer didn’t return — she jumped at the chance.
“My thinking was if something else came up I’d do it,” she said.
“For the next five years I was cancer free, but just as I was about to be sent off into the world a spot came back on my liver.”
Doctors removed part of her liver, but the cancer had spread to her pancreas by January 2016.
Ms Pickford thought she was running out of options until cancer-killing immunotherapy drug Keytruda came onto the Pharmaceutical Benefits Scheme (PBS).

A campaign by Professor Grant McArthur and business man Ron Walker, with the help of the Herald Sun, made the drug accessible for Australian cancer patients.
“Every three weeks I get an injection, straight into the veins,” she said.
“I needed (the drug) to work because of my family. I was really selfish and I wanted to see them grow up, so I put all my hopes, dreams and wishes into that drug.”
After about 11 months of treatment, doctors told Ms Pickford, now 35, she was cancer free.
“I’ll still be on Keytruda for the rest of my days,” she said.
Every three weeks Ms Pickford travels to Melbourne to have another dose of the “wonder drug”.
“Peter Mac are just amazing. My oncologist Dr Shahneen Sandhu has been amazing,” she said.
Ms Pickford warned others to be vigilant about getting sun spots checked.
“Definitely keep an eye out for any changes, it’s the changing (moles) that can get quite nasty,” she said.
‘I was told to wait till the end’
KERRY Duncan went from surviving breast cancer to being told it had turned into terminal illness in a matter of weeks.
Ms Duncan, 46, found a dimple on her breast, without a lump, in late September, 2015.
Test were done, including a mammogram and biopsy, which later found she had breast cancer.
Quick thinking doctors removed the 2.5cm growth but the worst was yet to come.
Five lymph nodes were removed as a precaution and one was cancerous.
Routine scans also found shadows on her bones — which concerned doctors at the time.
“They told me it could be arthritis or a birth defect and not to worry,” she said.
Ms Duncan said the worst day of her life when doctors told her she had stage four cancer.
“The doctors said: ‘The cancer has spread to your bones and there’s nothing we can do except keep you on the drugs’,” she said.
“I was pretty terrified and could not believe I was going to die from cancer.”
“I felt so well and considered myself to be really fit and healthy.”
Out of desperation, Ms Duncan’s sister Sally made inquiries about upcoming medical trials.
“Two days later I got a call about some research that was being done at Peter Mac,” Ms Duncan said.
Requirements were tight for the world-class medical trial but Ms Duncan was chosen as one of 15 people to be involved.
Ms Duncan received five rounds of a high-precision and high dose radiotherapy treatment and eight rounds of immunotherapy every three weeks.
Four months into the treatment Ms Duncan received the best phone call of her life.
“I was told there were no more signs of cancer. I was blown away,” she said. “I had to get him to tell me again.”
Ms Duncan said she’s ‘incredibly grateful’ to Peter MacCallum Cancer Centre for the second chance.
“I am so grateful they have an amazing team of people who do amazing work everyday,” she said.
“I feel like I have a second lease on life. I feel so lucky.”
Behind Melbourne’s incredible cancer breakthrough treatment
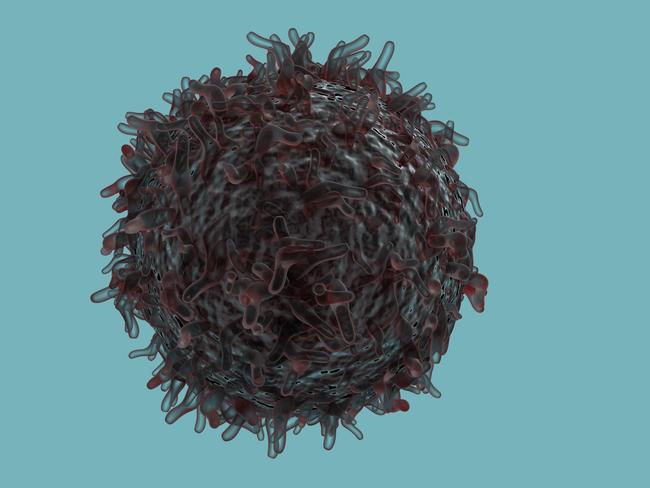
CANCER-killing cells are being taken from patients’ blood, re-engineered in a lab so they can seek out hidden tumours, and injected back into their bodies in the newest advancement in treatment.
The cutting-edge tailoring of the killer T cells is the latest evolution of immunotherapy, the new-generation cancer treatments promising to take over where surgery, radiotherapy and chemotherapy leave off.
In the most basic terms, immunotherapy is a new class of treatments that switch on a person’s immune system and convinces their own body to fight their cancer.
But since it emerged as a realistic treatment option over the last five years, immunotherapy has evolved so quickly that the number and complexity of cancers it is adapted to changes monthly — and Melbourne’s Peter MacCallum Cancer Centre at the forefront of the revolution.
Former Liberal Party and GP boss Ron Walker was one of the First Australians handed a lifeline through immunotherapy in 2013, and last year Hawthorn star Jarryd Roughead stunned the nation when his life was also saved.
But the latest advances are increasingly being used to save the lives of Victorians from all walks of life.

The Peter Mac now has 70 researchers working in eight laboratories focused on cancer immunology and immunotherapies, with a $7 million budget generated from national, international, state, industry and philanthropic sources.
The effort sees 45 immunotherapy clinical trials currently taking place at Peter Mac and through the VCCC alliance in Parkville, offering 140 patients a shot at next-generation treatments.
A further 170 patients are now accessing immunotherapies as standard treatments after they have passed the trial phase, with the hospital delivering about 400 treatments a month.
As she leads a world-first trial assessing the impact of immunotherapy on breast cancer, Assoc Prof Sherene Loi said the potential benefits were ever expanding.
“It is a paradigm shift,” Assoc Prof Loi said.
“Reactivating the immune system, in theory, has always been thought to give people a better chance of long-term survival from cancer. But we have only lately realised which part of the immune system is important.
“That is why this type of immune therapy has proved very successful and it is a game-changer, that’s for sure.”
While attempts to harness the immune system to fight cancer date back to the 1890s, the game-changing realisation came with the discovery of immune “checkpoints”.
Typically, when a virus infects a body the immune system responds by activating its killer cells to multiply and destroy the invader, before applying a brake so normal tissues are not damaged.
But cancer is different — it hijacks the checkpoint where the brake is applied and tricks the immune system into not attacking it.
With the immune system’s checkpoints uncovered, teams such as those at the Peter Mac are now developing a new class of drugs known as “checkpoint blockers” to remove the brakes.
A team centred on the ninth floor of the Victorian Comprehensive Cancer Centre are taking what may prove an even bigger step.
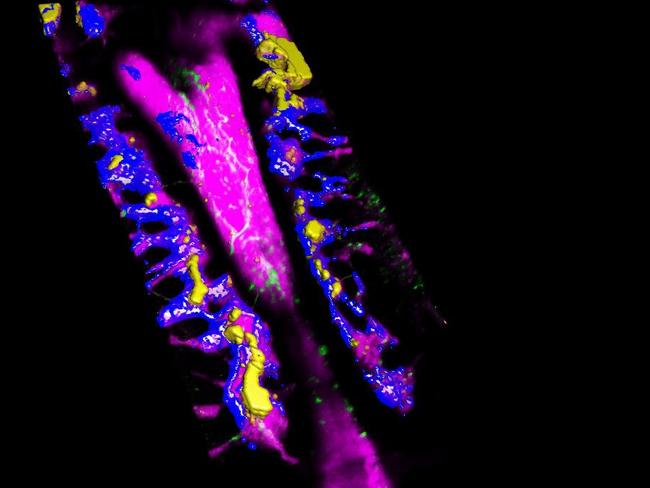
Late last year they launched a world-first clinical study that will see 30 Victorian patients have cancer-killing T cells harvested from their blood to see if they can be re-engineered to hunt down hidden cancers.
Once harvested, the patients’ immune cells will be cultured in the lab for 12 days while a gene is inserted that will prompt them to recognise the patient’s tumour, multiply and kill it, then set up inflammation so the immune system spreads.
Previously the re-engineered cells, known as CAR T cells, have only proven effective in overcoming advanced acute lymphocytic leukaemia.
But in a $9 million clinical trial funded by a major US-based Biotech company, the Peter Mac doctors will attempt to reprogram the killer cells to attack up to 70 per cent of cancers that all share the Lewis-Y antigen, including lung, uterine, breast, prostate, pancreas and colorectal cancers.
“It is like plug-and-play: you need to put an adaptor on the cell which you genetically engineer and now those cells, instead of detecting the leukaemia target, they detect the Lewis-Y which is the target on lung cancer, pancreatic cancer and so on.
“The cells were already in the patient but they were rudderless and couldn’t find the cancer.
“When the cells go back into the patient they have the means of detecting and trafficking to the cancer, and they are really angry and armed.”
Whereas immunotherapy treatments so far have been centred on convincing the immune system to attack tumours it already knows exist but ignores, CAR T takes it a step further and prompts the body to search and destroy a hidden disease it did not even know existed.
As one of the world’s foremost melanoma experts, Prof Grant McArthur knows the benefits of immunotherapy better than anyone.
It is in the killer skin cancer that immunotherapy had its first and, so far, widest use.
In the 1970s only one in three cancer patients survived five years, however improvements in surgery, chemotherapy and radiation therapy now see seven in 10 live — and up to 85 per cent for diseases which were previously fatal.
With immunotherapies still in its infancy, Prof McArthur believes it can radically improve survival rates further if matched with improved screening and early detection.
“I wouldn’t say there are no advances to be made in chemotherapy of radiation therapy, they could well occur. But they have been around for a long time and most of the improvements will be more incremental than radical,” Prof McArthur said
“We now have something entirely new, and that brings hope.
“We are now seeing of a reasonably regular basis astonishing cases of people that we thought were going to be bad, where everything turns around. It is remarkable.
“For melanoma we know the new treatments are effective even when there is microscopic cancer that you can’t see on a scan to stop it from progressing and relapsing — that is the next phase.
“If that goes really well, then we are talking about further big improvements.
“Can we eradicate those microscopic cancers even before we can see it on a scan like we do now chemotherapy in breast cancer now?
“That is the next wave of research, but the early signs are positive.”

Mother’s Day run for cancer research
The Women in Super Mother’s Day Classic is celebrating its 20th year this year.
The annual fun run, with events in every capital city and over 80 regional centres, has raised $30 million for breast cancer research.
Entries for the 2017 Mother’s Day Classic go on sale on Tuesday, and this year’s fundraising target is $4 million. Enter at mothersdayclassic.com.au


