Melbourne researchers develop ‘Fitbit for the brain’ epileptic seizure forecast implant
EXCLUSIVE: A “FITBIT for the brain” — an implantable device to monitor epileptic seizures and warn patients of impending episodes — has been developed in Melbourne.
VIC News
Don't miss out on the headlines from VIC News. Followed categories will be added to My News.
MELBOURNE researchers have developed a “Fitbit for the brain”, an implantable device to monitor epileptic seizures and warn patients of impending episodes in the hours and days ahead.
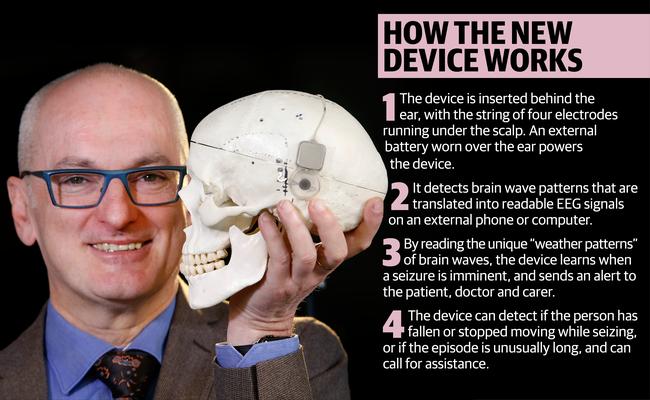
The world-first device aims to record and decode the unique “weather patterns” of brain waves. It would then send a phone alert seizure forecast, which developers hope will allow patients make lifestyle and treatment changes to increase their independence.
It has taken four years for the team of 100 neurologists, engineers, neurosurgeons and neuroscientists to create the device.
The St Vincent’s Hospital and Bionics Institute team is now negotiating with international manufacturers to produce a small batch of the devices for the first human trials early next year, a process that would cost $3 million.
St Vincent’s neurologist and director of the University of Melbourne Graeme Clark Institute, Professor Mark Cook said they wanted to keep the device in Australia to offer benefits first to those eligible of the 250,000 Australians with epilepsy.
“We’ve recently had some interest from private donors, which would potentially let us take this overseas to manufacture it. But if we could get an Australian manufacturer on-board we could put it into people very quickly and keep the know-how and jobs we’ve generated in Australia,” he said.
EPILEPSY TRIAL LEAVES VICTORIAN WOMAN SEIZURE-FREE
Prof Cook said the seizures were hard to diagnose given their infrequency, forcing patients on to trial-and-error of medications.
The device is inserted behind the ear and the electrode string runs under the scalp.
“It will help people manage their epilepsy better because they’ll be able to see how many seizures they’re having, whether a new medication has made a difference,” Prof Cook said.
“The phone will notify other people and call for assistance if they’ve fallen over with a seizure, or if it’s been going a long time. It could be for anyone; for the diagnosis of epilepsy or if they’re having blackouts and you’re not sure if they’re seizures.”
Other possible future applications could include monitoring electrical changes during sleep, measuring whether soldiers are conscious on the battlefield, and detecting changes in unconscious head trauma patients.
The device may help people such as 32-year-old new mother Georgie Frawley, who has endured serious medication side effects in an effort to control her grand mal and aura seizures.

While she is eligible for epilepsy surgery, that has a high chance of reducing her seizures, brain mapping studies have so far failed to conclusively detect where the seizures are starting.
“If my seizures were reduced I’d have more energy, I’d be happier, my husband would see a different person,” Ms Frawley said. “I just don’t participate in life anywhere near as much as I would if I didn’t have epilepsy, because I don’t know when the next seizure will happen.”


