It’s estimated 39 million people will die from antibiotic resistant infections between 2025 and 2050
Antibiotic resistant infections are a growing global threat that have already killed a million people every year since 1990. What can Australia do to fight them?

News
Don't miss out on the headlines from News. Followed categories will be added to My News.
Superbugs are set to kill more than 39 million people in the next 25 years, as experts warn the growing and “significant global threat” has already killed a million people every year since 1990.
Shocking new projections published in one of the world’s most prestigious medical journals, The Lancet, estimate 39 million people will die from antibiotic resistant infections between 2025 and 2050.
Under these figures, the annual death rate was tipped to rise by almost 70 per cent and researchers expect 1.91 million people – compared to 1.14 million in 2021 – to die directly from infections in the space of one year in 2050.
The paper also found superbugs’ impact goes far beyond fatal infections and estimated that – on top of the 39 million deaths directly from antibiotic-resistant infections – another 169 million deaths will be associated with them.
Once associated deaths were counted in the projections, estimates for 2050’s annual death rate reached a staggering 8 million.
Antibiotics’ discovery transformed healthcare, but different bacteria and other disease-causing pathogens that can resist the drugs have evolved over time, putting people at risk of contracting an illness that drugs can no longer treat.

Study author, University of Washington Institute of Health Metrics’ Dr Moshen Naghavi, said antimicrobial medicines were “one of the cornerstones of modern healthcare”.
“Increasing resistance to them is a major cause for concern,” Dr Naghavi said.
“These findings highlight that AMR has been a significant global health threat for decades and that this threat is growing.”
But the Global Research on Antimicrobial Resistant project’s modelling also showed exactly how tens of millions of lives could be saved – including with existing drugs – in the next 25 years, and called for urgent action.
The world could prevent 92 million deaths over the next 25 years by improving “overall infection care and access to antibiotics”, with South Asia, sub-Saharan Africa, and parts of Southeast Asia, East Asia and Oceania to benefit the most.
If researchers successfully developed a new antibiotic that could target gram-negative bacteria – some of the most resistant to antimicrobial drugs – another 11 million lives could be saved, the paper found.
Study author Norwegian Institute of Public Health and IHME affiliate professor Dr Stein Emil Vollset said while “real progress” had been made, “more must be done” before we lose eight million people a year in 2050.
“To prevent this from becoming a deadly reality, we urgently need new strategies to decrease the risk of severe infections through vaccines, new drugs, improved healthcare, better access to existing antibiotics, and guidance on how to use them most effectively,” Dr Vollset said.
The study found antibiotic resistant infections have decreased in children under 5-years-old thanks to major public health initiatives including widespread immunisation, and expect them to continue to do so, falling from 204,000 in 2022 to 103,000 by 2050.
But overall deaths will still increase rapidly due to spikes in other age groups, particularly people aged over 70 – where numbers are expected to more than double.
Study author University of California Los Angeles and IHME affiliate professor Dr Kevin Ikuta said the fall in deaths among young children in the last three decades was “an incredible achievement”.
“However, these findings show that while infections have become less common in young children, they have become harder to treat when they occur,” Dr Ikuta said.
“Further, the threat to older people from AMR will only increase as populations age. Now is the time to act to protect people around the world from the threat posed by AMR.”
The GRAM project based their projections on more than 520 million individual records – including hospital data, death records and antibiotic use data – and spanned all 204 countries and territories.
The researchers said their study did have limitations, including a lack of data from some low and middle income countries, and that some of the 520 million records they relied on could have contained inaccuracies.
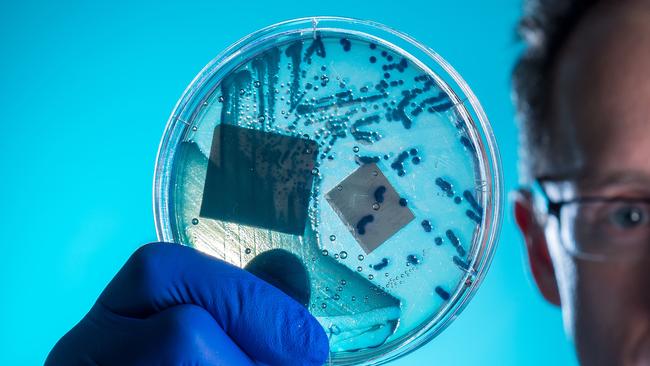
The GRAM project includes multiple global bodies, including Australia’s CSIRO, La Trobe University, Monash University and more, and was funded by the Wellcome Trust and UK Government.



