Hundreds of millions needed to fix Victoria’s broken health system
Sick patients are being treated in hospital hallways, waiting areas and ambulance bays amid Victoria’s health crisis, with experts warning the system will collapse without a significant funding boost.

Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Victoria’s health system is at breaking point with the state and federal governments facing urgent calls to find hundreds of millions of dollars to save it.
Ahead of next month’s state budget, leading health agencies and experts have warned that without a significant funding boost the system will collapse.
Treasury officials are currently working on plans to slash funding to services in a bid to rein in spending and curb the state’s worsening debt path.
Official forecasts currently project net debt to grow to a record $188bn – or $72,000 per household – by 2028.
But senior government sources said that figure would almost certainly blow out when Jaclyn Symes hands down her first budget on May 20.
MPs have been warned to scale back requests for electorate funding while ministerial proposals are being carefully scrutinised.
Latest submissions to the parliament’s inquiry into Ambulance Victoria, which were published this week, warn the health system is on the verge of collapse.

The Australian Medical Association warned that a chronic shortage of hospital capacity was contributing to ambulance ramping and workforce burnout.
“The consequences of ambulance ramping and access block extend beyond ambulances waiting outside hospitals,” it said.
“Paramedics, emergency physicians, and other hospital-based staff, are operating in a high-pressure, unsustainable environment, managing an unrelenting influx of patients while navigating administrative inefficiencies, workforce shortages, and limited resources.
“Many emergency physicians now routinely provide care in hallways, waiting areas, and ambulance bays, simply because inpatient beds are occupied by patients who could be discharged if appropriate community-based services were available.
“Corridor medicine has become routine, with patients receiving treatment in hallways, waiting areas, and ambulance bays while staff struggle to free up beds. These delays pose direct risks to patients experiencing strokes, heart attacks, or traumatic injuries, where every minute is critical.”

The AMA argued that without “decisive intervention”, ramping would worsen and emergency response times further deteriorate “further crippling the system”.
According to its latest public hospital scorecard, the annual percentage increase in federal funding has decreased from 2.39 per cent to just 1.83 per cent.
At the same time Victorian government investment as increased from 4.35 per cent to 9.42 per cent, with 67 per cent of funding coming from the state government – significantly higher than the national average.
Health policy adviser, adjunct Associate Professor Ray Bange, said government funding of Ambulance Victoria needed to be increased by at least $300m in this year’s budget.
He also called for the Allan government to negotiate an amendment of the National Health Reform Agreement with the Commonwealth to provide funding for Ambulance Victoria either fully or on a dollar-for-dollar basis, matching the contribution of the state.
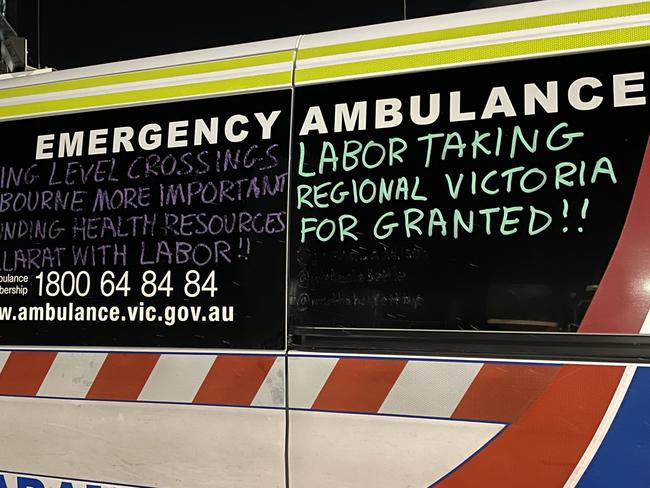
In its submission the Victorian Ambulance Union repeated warnings that one fifth of paramedics were considering leaving the job.
“Morale is currently the lowest I have ever seen it during my time with the organisation,” one paramedic said.
“Bold, progressive, decisive leadership and decision making at a high level within government and Department of Health is rapidly required to shift AV away from being the metaphorical scaffolding that is currently propping up all areas of the failing healthcare system.”
The inquiry has been told that in the period between January 2018 and September 2023, emergency ambulance and patient transport crews spent a cumulative 120 years, or 523,000 hours, waiting for their patients to be admitted to hospital.
Ambulance Victoria’s total revenue increased from $729m in 2014-2015 to $1.48bn in 2023-2024.




