Game changing new test can predict a child’s risk of developing chronic type one disease
Every child may soon be screened for type 1 diabetes after researchers discovered a simple test to diagnose who is at risk before symptoms appear.

Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Melbourne researchers are on track to screen every child in Australia for type 1 diabetes after finding a simple test to diagnose who is at risk of the chronic disease before symptoms appear.
Experts from the Royal Melbourne Hospital and Walter and Eliza Hall Institute of Medical Research found a single finger prick test – taken two hours after a glucose drink – could determine who was likely to develop the disease and how quickly. It was just as effective as the current protocol of five blood tests.
The screening test would allow doctors to closely monitor those children, and to act on the disease at the earliest opportunity.
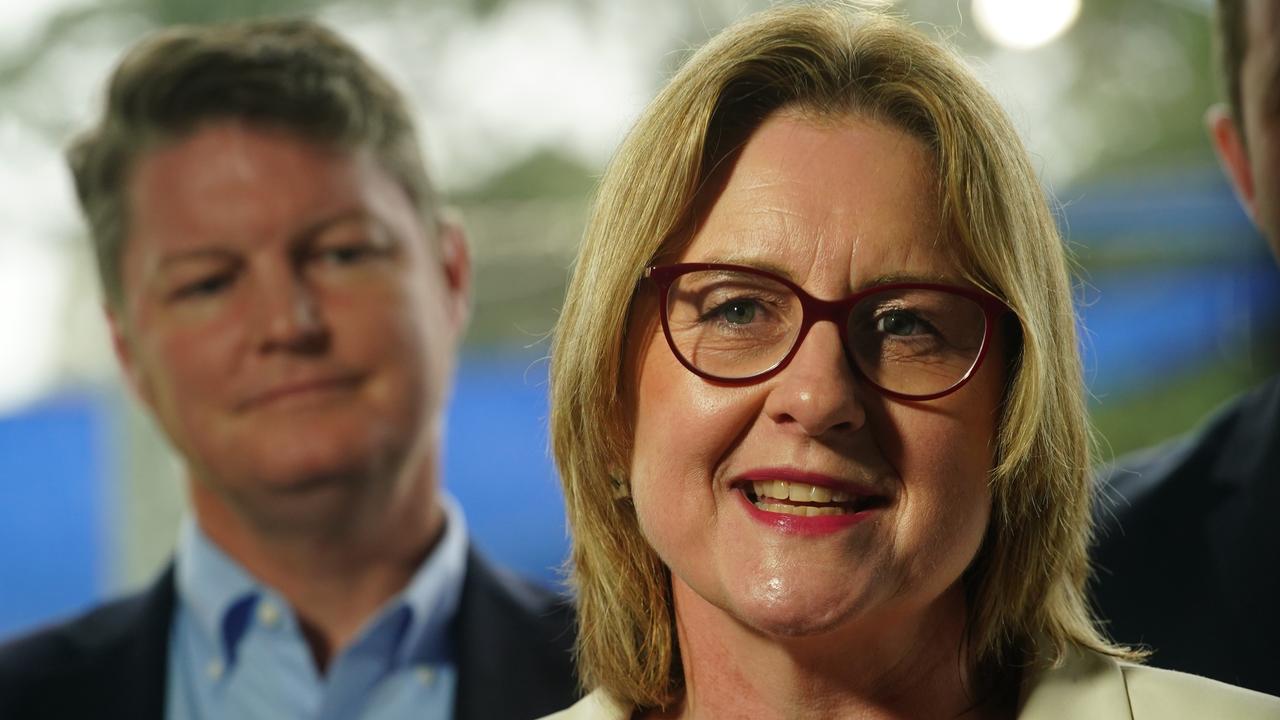
Lead researcher and endocrinologist Associate Professor John Wentworth said their validation of the blood test in people with diabetes-related antibodies, was an “important piece of the puzzle” in determining who could benefit most from early intervention.
“Ultimately we have bold visions for not only testing every kid in a diabetes family, but every kid in Australia,” Prof Wentworth said.
“That’s because the vast majority don’t have family members with type 1 diabetes. Just about 10-15 per cent have a family member with diabetes.”

“The whole ecosystem hinges on our ability to find people at risk. Lots of delayed diagnoses happen in kids, and that’s why they get sick. We really want to pick when they’ve started to go off.
“We need a good way of making the call; who is at most risk of going quickly to needing insulin, and who are we less concerned about. That’s what this test will do.”
The first stage of diabetes screening currently looks for chemical markers in the blood – called islet autoantibodies – that act as the signposts of the silent auto-immune processes taking place.
These markers can circulate for months or years before symptoms appear, but not everyone who has them will go on to develop the disease.
Those with antibodies then undergo several blood tests taken during a “glucose tolerance challenge” to further confirm the diagnosis.
But this new cheap and less-invasive finger prick test would replace it – and it could also play a key role in a population-based screening program.
It would allow children to receive immunotherapies, which have been shown by these same Melbourne researchers to delay the onset of type 1 diabetes – otherwise known as juvenile diabetes – for at least two years.
Researchers hope children could also receive treatments that turn off the immune attack on the pancreas before irreversible damage occurs, essentially stopping diabetes in its tracks.
“By the time people turn up to hospital needing insulin, that’s too late,” Prof Wentworth said. “They’ve lost too much of their pancreas.
“This test could help you track kids over time.
“You could set it up routinely, and potentially even do it in the home.
“We are working up the methodology for that.
“We need to screen to find young kids who are at risk and work out when they should be put into a study to use immunotherapy to treat it.
“Insulin was transformational when it was discovered a century ago and has prevented kids dying, but we reckon it’s held us back quite a long way because we’ve developed this whole treatment mentality where insulin is the best thing and the only thing.
“The reality is we think we can do it without insulin if we find kids early enough, and if we’re smart with how we give them immune therapy to turn off that immune attack damaging the pancreas. That’s the latest challenge for the field.”