Baker Heart and Diabetes Institute shows drug can ‘re-wire’ insulin production in diabetics
In a world first, Melbourne researchers have found how to “rewire” insulin production in people living with diabetes. Here’s why it’s a life-changing discovery.
Victoria
Don't miss out on the headlines from Victoria. Followed categories will be added to My News.
Melbourne researchers have found a potential cure for diabetes, describing it as a “serendipitous” discovery.
Lead researcher Professor Sam El-Osta said the groundbreaking therapy “rewired” insulin production in people living with diabetes.
It has been achieved using two drugs already approved for use in the US for rare cancers.
Professor El-Osta led the team from the Baker Heart and Diabetes Institute and said it was “life-changing research”.
“The method we have developed rapidly restores insulin production in pancreatic cells that have been destroyed by diabetes,” he said.
Professor El-Osta said the therapy could harness a diabetic patient’s remaining pancreatic cells and potentially modify the course of diabetes and eliminate the need for insulin injections.
“It is world-first, proof of concept in human research originating in Melbourne, showing pancreatic regenerative capacity by harnessing the patient’s remaining cells to increase the production of insulin,” he said.
“What we are interested in is a cure.”
The Baker team published the results of the study overnight in the scientific journal Nature.
The researchers revealed the drugs, not originally designed or licensed for the treatment of diabetes, rapidly regenerated insulin in pancreatic stem cells in human donors.
The lead authors of the publication, Dr Keith Al-Hasani and PhD student Safiya Marikar, used pancreatic cells from a child and also adult type 1 diabetic donors, and also an adult without diabetes. They showed that just 48 hours of stimulation with the drugs restored insulin production from damaged pancreatic cells.
Professor El-Osta says the therapy also overlaps with type 2 diabetes and could be used for the 30 per cent of people living with diabetes who will eventually rely on insulin injections.
He says the potential of the world-first discovery is exciting.
“What we have been able to do is harness the patient’s remaining pancreatic stem cells, despite the absolute destruction of the main machine that produces insulin, the beta-cell,” Professor El-Osta said.
Beta cells are the cells that make insulin and are found in the pancreas.
He says while pharmaceutical options, such as injectable weight loss drugs like Ozempic, are fantastic at lowering blood glucose levels, they do not prevent, slow or reverse the destruction of the beta-cell.
“The beta-cell is the first casualty in diabetes and injectables don’t slow down, nor do they reverse the decline and destruction in insulin-producing beta-cells,” Professor El-Osta says.
“That is key to our clinical research. We think we are five years away from potentially having a disease-modifying treatment for type 1 diabetes.”

He told the Herald Sun the research was leading the way with a potential cure and also showcased how to bridge the gap between research and industry partners to translate therapies from humble beginnings and bring them to an international level.
“We have been working on this for seven years, with work funded by the National Health and Medical Research Council in Australia and the Juvenile Research Foundation in New York,” Professor El-Osta said.
“We have now engaged in discussions with commercial and industry partners to take this forward.”
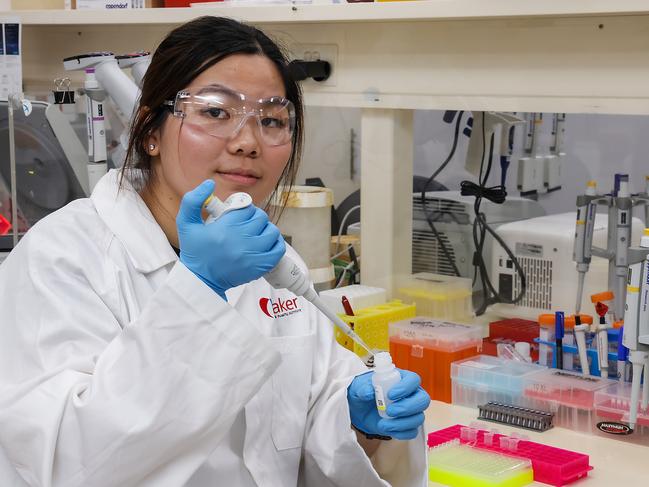
The team at the Baker also includes Chin Jin Ker who is helping to lead the research. For her it is personal.
Dr Ker was diagnosed with diabetes when she was 12 and now wears an insulin pump. She describes diabetes as an exhausting, chronic battle. “It is also invisible,” Dr Ker said.
And while grateful for the pump device that delivers automatic doses of insulin around-the-clock that she says has “made her life so much better”, Dr Ker adds it is not a solution.
She hopes the team’s discovery can be.
While organ transplants for people living with type 1 diabetes have proven useful, the stark reality of donor organ shortage has limited widespread use.
“Our research addresses this unmet medical need,” Professor El-Osta said.
Diabetes at a glance:
• Diabetes is an auto-immune disease where blood glucose, the body’s main energy source, is too high.
• Treatment can include daily insulin injections, insulin pumps or a pancreas transplant.
• It affects around one in 20 Australians and occurs in both children and adults with the causes not well known
• This is the first time a drug has been found to “rewire” insulin production in people with diabetes




