Parkinson’s surgery now lets patients sleep through procedure
THOUSANDS of Australians with Parkinson’s disease could soon undergo life-changing surgery to control tremors and stiffness while asleep on the operating table for the first time.
News
Don't miss out on the headlines from News . Followed categories will be added to My News.
THOUSANDS of Australians with Parkinson’s disease could soon undergo surgery guided by their own brain signals without having to be “awake” on the operating table, after a breakthrough finding by Melbourne researchers.
The Bionics Institute team has found the signature of brain activity that ensures they have placed the electrodes in the millimetre-perfect position in the brain — their target the size of the tip of a grain of rice — that will allow Deep Brain Stimulation for the progressive condition to no longer necessarily be performed as “awake” surgery.
Allowing the patient to sleep removes the anxiety that now stops many undergoing the procedure.
WATCH HELPS MONITOR PARKINSON’S DISEASE
NEIL DIAMON CANCELS TOUR DUE TO PARKINSON’S DIAGNOSIS
DRUGS FOR GHRELIN HORMONE COULD PROTECT AGAINST PARKINSON’S

The biomarker finding, a major breakthrough for the field of DBS, is also tipped to shorten the trial-and-error process of finding the right settings of electrical stimulation for each patient to best reduce their tremors, stiffness and jerkiness.
After four years of research and three years of testing at the Austin Hospital, St Vincent’s and St Vincent’s Private, the finding is also a giant leap forward for the field searching for the “holy grail” treatment for Parkinson’s — a closed-loop system that turns the stimulation on and off in real time in the patient’s brain in direct response to the patient’s instant needs.
About 10 million people have the incurable disease globally — including about 100,000 Australians — with 10-20 per cent of them estimated to be candidates for DBS at some point. But lead researcher and neurologist Dr Wesley Thevathasan said only a small fraction of those eligible patients choose to undergo the procedure.

“At the moment, patients have to go through awake surgery to insert the electrodes and, even if they may benefit from it, it’s just too anxiety-provoking for a proportion of patients,” Dr Thevathasan said. “This surgery has been around for 20 years, and one of the disappointing things is that so little has changed over that time.
“That’s why this development is of great importance, because it can shift the whole field forward; making a good therapy better, and teams who do a few cases to be almost as good as those who do a lot.”
The finding means an extra 9000 to 17,000 Australians could benefit.
The Bionics Institute team is also led by biomedical engineers Nicholas Sinclair and Hugh McDermott, and neurosurgeon Kristian Bulluss.

DBS for Parkinson’s has been around for 20 years and has been offered as a standard of care for the past decade.
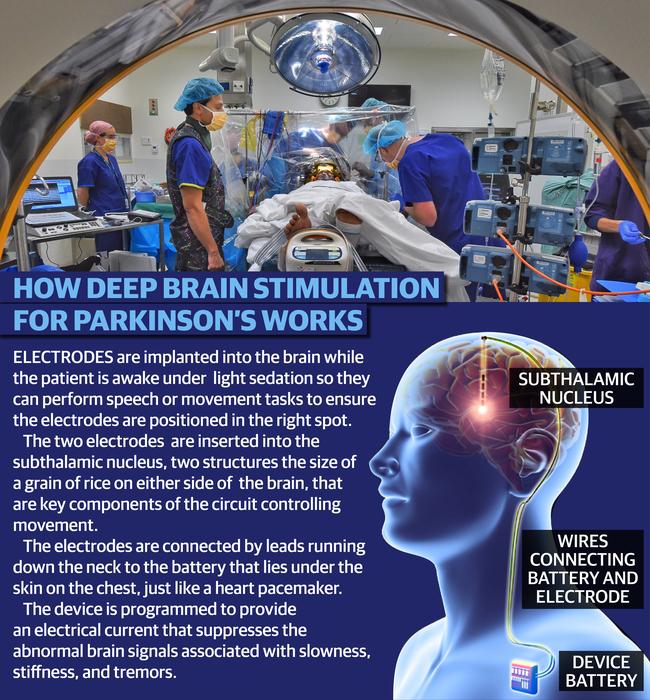
Electrodes are implanted into the brain under 3D computer mapping guidance while the patient is awake, but under light sedation, so they can perform speech or movement tasks to help ensure the electrode tip is positioned millimetre-perfect.
Other research groups around the world have been looking for a biomarker, to confirm the electrode’s correct position in the subthalamic nucleus, based on “spontaneous” brain activity that is continuously happening.

But the BI team looked at what the brain was doing in response to the electrical stimulation.
They found this signal of voltage that occurs in brain cells after a pulse of stimulation was an effective biomarker. In 14 Parkinson’s patients and five with Essential Tremor, they found that the stronger the signal, the closer the electrode was to the correct spot in the brain.
The team then followed patients up over three months later, finding that patients had the best response from the treatment when it was applied where the biomarker signal was strongest.
The findings were published today in the journal Annals of Neurology.
The team now is seeking funding to run a clinical trial testing the technique in comparison with standard awake surgery, before it could be offered globally as the preferred option.
NO TREMOR, I’M WAY IN FRONT - by Geoff Wilkinson
MORE than 2000 Australians with Parkinson’s disease have been wheeled into operating theatres to lie wide awake while holes were drilled through their skulls and tiny electrodes implanted deep in their brains.
I was one of them and, quite frankly, I would have rather been unconscious while the Deep Brain Stimulation surgery was performed.
But my experience is the perfect illustration of why a world-first breakthrough by Melbourne specialists in the treatment of Parkinson’s is so important.
No longer will patients have to be awake for the first half of a four-hour operation, so they can respond to questions and directions which enable neurologists to be sure they’ve hit the right spot, which is in the subthalamic nucleus area of the brain and is the size of the tip of a grain of rice.
In my case, the first of two probes through the skull and into the STN was a bullseye, but the second wasn’t. The experts knew it wasn’t because my face had sagged like a stroke victim, my eye on the same side was twitching constantly and uncontrollably, and I felt horribly ill. Lying there, fully conscious, listening to my neurologist, Wes Thevathasan, and surgeon, Kristian Bulluss, discussing Option B was not one of the highlights of my life so far.
Fortunately, the back-up plan was a success and so was the operation.
I was diagnosed with Parkinson’s more than 10 years ago, when I was told the disease was “chronic, progressive and incurable”.

Parkinson’s is an insidious, creeping, condition. It is often not obvious for several years after diagnosis but then, gradually but inexorably, it affects your quality of life and your ability to perform what used to be simple, routine tasks. It affects your mobility, dexterity, strength and balance, and causes shaking, shuffling, salivating, restless legs and a deterioration in various other bodily functions you used to take for granted.
Against the odds, holistic therapist Antonia Ruhl slowed my most severe symptoms for more than a decade. But, inevitably, the battle was being lost. I had little to look forward to when I had my first appointment with a new specialist, Dr Thevathasan, on August 15, 2016, and he asked if I’d considered DBS.
I hadn’t but within three months, I’d done my due diligence, spoken to five others who’d already had DBS and was ready to face the music (Van Morrison, because the patient gets to choose). Now, 17 months after the operation and 12 months after tracing my grandfather’s heroic footsteps along the Western Front in World War I, my quality of life has improved dramatically and I’m a long way in front in terms of risk versus reward.
I still have Parkinson’s, but I also have two part-time jobs and a book to write.

I have no tremor and I’m taking no medication, which means I’m no longer captive to the pills that rule the lives of Parkinson’s sufferers. I enjoy boxing, folding socks, doing up buttons and pulling on a jacket unassisted — all tasks that used to be beyond me.
My condition has improved to the point that the electrical stimulation levels from the transmitter implanted in my chest now match the best state I could have achieved on medication — but at a constant level, rather than being tied to the peaks and troughs and side effects of the pills. Dr Thevathasan says stimulation levels will no longer be a matter of trial and error or guesswork when the new signal starts communicating with the brain.
Not only will the electrodes be in exactly the right place, with pinpoint precision, but the brain will give feedback about how much stimulation it should be receiving. The brain’s stimulation levels will be monitored and updated every fraction of a second, and the levels will be automatically adjusted if and when required.
The lucky 2000 Australians who have to recharge their batteries once a week and may need a new DBS transmitter to take advantage of this amazing discovery are perfectly placed to understand its extraordinary potential.
Hopefully, the $10,000 donated by my family and friends for the privilege of seeing me without my (very) old grey beard before the operation has in some small way helped fund Parkinson’s research. I may be battery-driven, but the future looks brighter than it did last week.
I reckon I can see the light at the end of the Subthalamic Tunnel.


