Surgeons push for public funding boost for weight-loss surgery
LEADING surgeons are pushing for a massive increase in publicly funded weight loss surgery to make it a frontline treatment not only for obesity, but also other killer lifestyle diseases.
News
Don't miss out on the headlines from News . Followed categories will be added to My News.
LEADING surgeons are pushing for a massive increase in publicly funded weight loss surgery to make it a frontline treatment not only for obesity, but also other killer lifestyle diseases.
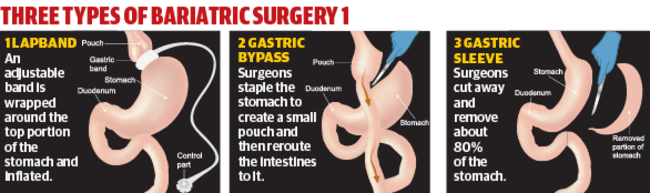
While the number of bariatric operations in Australia has doubled in just seven years, public patients are still struggling to access the surgery capable of saving them — and the Australian economy — from chronic heart disease, diabetes, joint replacements and other complications of their size.
A new analysis of weight loss surgery data shows the few people who do get taxpayer-funded procedures have waited years longer and become fatter and sicker than those who can pay.
Of the 22,000 Australians to have weight loss surgery last year, only 7 per cent received any public funding from Medicare — and only 4 per cent were fully funded.
Prof Wendy Brown, who oversees Australia’s Bariatric Surgery Register, said the lopsided situation discriminated against those in the greatest need.
JUNK FOOD TV BAN TO SAVE KIDS FROM OBESITY
CUT CARBS, BOOST FATS TO AVOID OBESITY
OBESE PATIENTS A DRAIN ON REGIONAL MEDICAL CARE
RAIDING SUPER TO PAY FOR OBESITY SURGERY COULD BE STOPPED
“It is becoming urgent that we look at a way to improve access to people, because this is a viable treatment option that has a good evidence base and the opportunity to change people’s lives, yet large numbers of people are excluded from it,” she said.
“It is not just weight loss surgery, it is health giving surgery.”

The register’s data shows private patients are typically female with an average age of 43 and a BMI of 43, and 15 per cent have diabetes.
The situation is much more severe for the few public patients.
They have an average age of almost 50, a BMI of 50 and an almost a third have diabetes.
For both groups the benefits of surgery are huge — on average patients lose and keep off the half to two thirds of the extra weight they were carrying, with rates of diabetes, liver disease, joint damage, heart disease and fertility all vastly improving.
The health system also benefits by avoiding decades of Medicare-funded chronic disease treatments.
The cost of managing diabetes is almost $15,000 a year for each patient — while obese Australians also have 70 per cent higher rates of cardiovascular disease, 88 per cent increased chance of osetoarthritus that can require hip and knee replacements, as well as greater rates of several cancers.
The Royal Australasian College of Surgeons has issued a paper calling on governments to step up publicly-funded bariatric surgery, which vice president Cathy Ferguson said was overdue.
“We certainly support equity of access for publicly-funded weight loss surgery,” she said.
The Australian & New Zealand Metabolic and Obesity Surgery Society is calling for urgent action.
As well as becoming a frontline treatment for obesity, ANZMOSS president Mr Ahmed Aly said bariatric surgery should be offered to combat diabetes, hypertension, liver disease and other obesity-related conditions.
“When you factor in that the people most affected are the lower socio-economic classes, and they have less access, this is something that has to change,” he said.
“This is good treatment that has significant health benefits, it saves lives, it has an economic benefit, and we are not using it.
“We all love the concept of Medicare and equal access, but obesity surgery simply is an area that has not kept up.
“We are nowhere near what’s required in the public system.”

‘IT GAVE ME A CHANCE’
SURGERY was certainly not a silver bullet for Mark Haldane, but it did give him the headstart he needed to overhaul his life.
Four years ago Mr Haldane was almost 150kg, pre-diabetic, unable to exercise to improve his health and warned he would be dead within 15 years.
Now he is less than 100kg, runs 50km a week, loves martial arts and does not have diabetes.
He has also turned 50 and is looking forward to a long and healthy life, thanks not only to his bariatric surgery, but the hard work it allowed him to put in so he could make the most of it.
“My doctor basically said get off your a---, go do something or you won’t make 55-60,” he said.
“I thought, ‘who is going to look after my wife?
“This (surgery) isn’t a fix, this is a start.
“Within 12 months I had lost 40kg, which meant I could start exercising, living and changing my lifestyle.
“When you are 140-160kg you can’t just go for a 5km walk — even tying your shoelaces is hard.
“Once I started losing weight I started walking and, it might have been only walking around the block, but it meant I could.”
While Mr Haldane could afford to pay for his lifesaving surgery, he has grave concerns for others who need the same chance even more than he did.
“I have a friend who has significant weight issues and he can’t afford private health ... I don’t think he will make 60, in fact I don’t think he will make 50, and he is only in his 40s now,” he said.
“The cost of looking after someone with diabetes and high blood pressure and all the other issues that go along with obesity is astronomical.”

BUT MY OPERATION WAS A NIGHTMARE
WHEN Anita Carmel underwent weight loss surgery it was a “last resort” bid to shed the kilos she had piled on after earlier botched emergency surgery.
A bout of depression and binge eating in the two years after nerve damage left her disabled with foot drop, saw the former customer service worker’s weight balloon to 135kg.
Although Ms Carmel now weighs 95kg, she has paid a horrific price for her near fatal decision in late 2015 to undergo gastric bypass.
A post-operative collapse at home saw the then 33-year-old spend seven weeks in hospital with an obstruction, gangrene and perforation of the bowl. In that time she underwent a further four operations including a laparostomy and the removal of a large proportion of her bowel and other infected tissue. Almost five months of in-home care followed.
Complications from bariatric surgery have caused six deaths in Australia, with the cause of death still to be determined in 11 other cases where patients died after weight loss surgery.
Ms Carmel said she knew she was in serious trouble when her sister travelled from her home overseas to be by her bedside.
“I was trying very hard not to think about (whether I would survive). I was trying very hard to keep my mind off that sort of stuff,” she said.
“I was just trying to get home, I was in pain, I was uncomfortable. It was so painful to sleep on.”
The ordeal has left Ms Carmel terribly disfigured, with a 14cm x 14cm scar, and eaten up the disability pensioner’s meagre savings.
“It’s horrific. It’s still numb,” she said of her abdomen. “I actually have no feeling in that area at all. It is also on a diagonal so my belly button is a fraction of the size it was extremely lopsided.”
Even after her ordeal, Ms Carmel’s weight stubbornly remains 25kg above her desired healthy level, as she shed little more weight since leaving hospital.
Ms Carmel is now suing her surgeon.
Her lawyer, Slater and Gordon medical negligence team associate Awash Prasad, said the toll on the mental wellbeing of patients who suffer poor results from weight loss surgery can be dramatic given the motivation for undergoing such surgery is to look and feel better.
Mr Prasad said too often doctors fail to go beyond listing possible risks to patients, and advise them of the potential short, medium and long-term complications and the strategies in place to detect and deal with such complications should they arise.
“In Anita’s case, for example, the only thing that was required was what’s called an oral contrast and a CT scan day one post-operation,” he said. “That is a plan that was not in place and did not take in effect. If that was done they would have picked up that she had a bowel obstruction and they could have repaired that and she wouldn’t have had to go through what she did.”
One in 40 patients undergoing their first bariatric surgery suffer a complication — a similar risk of complication or death as gall bladder surgery.
Complications are far more frequent for those who require additional surgery to repair or replace a previous bariatric implant, with one in 16 patients suffering a complication.
Fatal complications have included leaking staple lines, leaks leading to organ failure, a fistula track and sepsis infection.
Professor Wendy Brown, who oversees Australia’s Bariatric Surgery Register, said there were risks with all surgery and weight loss surgery was “remarkably safe” compared to other forms of surgery.

“It is incredibly safe surgery when you consider the patient population we are operating on,” she said. “Often people have other problems like diabetes ... there are lots of other illnesses that go along with their surgery than can make it less safe.”
In a writ lodged in the County Court, Ms Carmel alleges that before sending her home her surgeon failed to properly investigate the cause of her continuing pain, persistent nausea, vomiting and retching, or inability to tolerate oral fluids or pass a bowel movement.
“I was quite nervous about (going home) because I was being sick with everything,” she said.
“I also wasn’t tested, he didn’t do any scans, he basically told me that it was normal after an operation for me not to keep anything down.”
“I wasn’t 100 per cent confident about that but I took his word for it because I was told he was the best in his field so I trusted him.”
Ms Carmel said the she spent the next few days until her first check up at home but could still not keep anything down, and was extremely unstable on her feet.
“Every time I stood up I felt like I was going to collapse. Even walking down the hallway for his appointment I almost collapsed,” she said.
“He asked to see the site where he put in the instruments and the cameras and I actually fell back into my chair; and he still sent me home.”
Later that night Ms Carmel collapsed and called her family who told her she should go to hospital as something was clearly very, very wrong.
Between undergoing scans, Ms Carmel said she was about to tell staff there was a foul rotting smell in the bathroom “when I realised it was actually me”.
The scans revealed she was suffering a bowel obstruction and her wounds and strangulated hernia were badly infected.
Ms Carmel claims her surgeon was negligent in failing to consider the possibility of bowel obstruction or undertaking appropriate scans and tests. In addition to her physical injuries, she claims she has suffered anxiety and depression and suffers ongoing gastric issues, and even has to pack her now tiny belly button with cotton wool to prevent it rubbing raw.
Ms Carmel said a payout would help her pay for plastic surgery, visits to a psychiatrist and ongoing specialist medical treatment.
“My weight loss has plateaued so I don’t know if it was successful in that aspect because I haven’t actually lost any more weight which I am very concerned about. I also have this enormous and extremely hideous scar on my body which will be there permanently unless I have plastic surgery.
“I have a lot of emotional issues around this that I haven’t been able to sort out because I can’t afford to.”
Ms Carmel warned others considering weight loss surgery that it should never be their first choice and to find out what the risks are.
“Don’t automatically think that it’s going to be the be-all-end-all ‘save you’ solution.”
- Peter Mickelburough


