Why Royal Children’s Hospital top ICU doctor Warwick Butt is not panicking over COVID-19
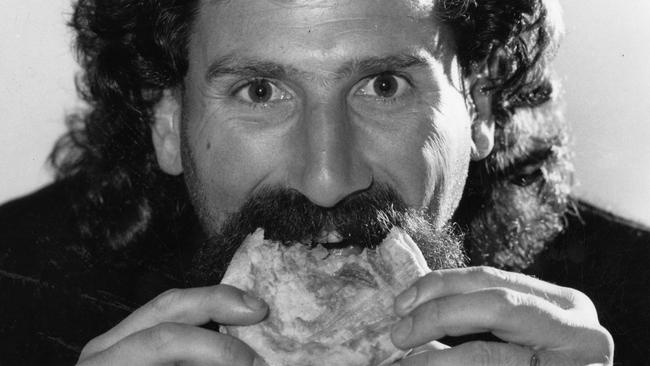
The coronavirus crisis has sown chaos globally, but this ICU top doc says “it’s business as usual” at his Melbourne unit. This is why Dr Warwick Butt isn’t panicking — and when he thinks footy will return.

Coronavirus
Don't miss out on the headlines from Coronavirus. Followed categories will be added to My News.
I was told by a smart doctor that one of the best people to speak to about COVID-19 was here in Melbourne.
Warwick Butt started off doing paediatrics in the late ’70s, working in neonatal intensive care before moving to Toronto.
When he came back to Melbourne, he started work as a paediatric intensive care specialist and was also a part-time paediatrician.
Warwick worked at the Alfred in adult intensive for about 16 years, before shifting to the ICU at Cabrini, where he now works part-time. He still works full-time at RCH.
PARTYGOERS, BIKIES CAUGHT OUT AS CASES SPIKE
BEST FITNESS APPS TO TRY IN SELF-ISOLATION
HM: I was told you are often the smartest guy in a room but do people always agree with you?
WB: I am speaking to you on the understanding that these are personal views and in no way represent the opinions of any organisation I may be associated with and also that there are many very talented clinicians who will probably disagree!
HM: Are you related to Robert DiPierdomenico?
WB: Ha ….no, Dipper is much braver and more athletic than me! Different genes!
HM: We live in strange times – how much of your week at the moment is dealing with, seeing, discussing, COVID-19?
WB: About 3 hours a day, six days a week.
HM: When was it that you first heard about COVID-19?
WB: In a serious way, early February.
HM: When did you think, “this will change the way we live and shape our lives dramatically?”
WB: Pretty much straight away. We knew immediately it would have a huge impact as a new virus without a vaccine.
HM: What were the early discussions?
WB: How to best deal with it when it eventually came to us.
HM: Were there varying opinions?
WB: There are two options of dealing with COVID-19 which I’m sure you’re aware of. There’s the flatten the curve approach, and then there’s the mountain approach which is what has happened initially in America and Italy. We knew each approach had good and bad parts to it. Ultimately, we felt that Australian government would choose the flatten the curve. We started planning for how we at RCH and ICU could best manage. In mid-February, in ICU we developed two guiding principles early on, which set the baseline for everything we did. Number one: We just do the best we can for each child in the normal way. Number two: everything we do has to be done in a way that protects the staff. Having those two key principles made the second half of February, March, and now April, easy.
HM: Since making those early decisions, has it played out as expected?
WB: The biggest problem for us was the fear and panic that was generated around the world. I’m not trying to make light of the disasters that evolved in New York, Italy and the UK, as they were countries that we related to, but we felt that as the chaos evolved, there was anxiety setting in everywhere. You could sense and feel it in the flooding of information across the internet. Everyone wanted to share every bit of information, but most of it was repeated, alarming, and premature.

HM: How did we avoid panic?
WB: Good people across the country in the health system kept calm, we knew we had time to prepare. We established a diverse leadership group with people who had really good expertise that were a part of the intensive care unit. The leadership group was able to interact with different aspects of the hospital, and instead of our people going on email and putting out an email for 150 people, you had to go through the leadership group first. We would then tweak it, respond to it, and then deal with it in an organised way. It also meant our messages were generally consistent.
HM: And as a result of that process?
WB: The reason I missed your call earlier was because I was walking around the ICU asking the team we have” “How do we feel – how are we coping?” The answer from almost all was: “Good – it’s business as usual.” There’s no panic. In the middle of an average winter when we have five or six patients above our normal number, we’re stressed and anxious. As of today, it’s just another normal day at work, normal numbers in beds, so it’s really worked well and we are in good shape.
HM: Just to rewind a little – how did COVID-19 actually start? You hear that someone in China ate an animal that was infected with it. Is that fact?
WB: That’s what everyone is saying happened, and that’s what a couple of world-famous infectious disease doctors are supporting. For conspiracy theorists, there is a lovely conspiracy. Of course, Wuhan is where the genetic, biological warfare centre of China is. Where the market is would be a very easy place to release something, and see what happened China got on top of it quickly. They had resources. They may have been prepared because of the SARS virus, which was also a coronavirus, so they may have been better prepared than the rest of us, but they seemed to handle it in an incredibly organised, systematic way. The conspiracy theorists will go with that, and the others would believe that the animal had it, gave it to the bat and the bat gave it to the humans when they ate it.
HM: SARS was a coronavirus? I didn’t know that.
WB: Yes – the coronavirus has a crown like shape to it – hence “corona”. There are lots of strains of it.
HM: When people say “it’s not much more dangerous than the flu”, what is your response?
WB: They aren’t completely wrong. In the United States, last year there were 38 million cases of the flu, and there were around 80,000 deaths with more than 500,000 admitted to hospital. Did you hear anything about it?
HM: No.
WB: There’s more than 500,000 cases of coronavirus in the US, and 32,000 deaths. Terrible but not like last year; so, we have to try and keep calm and rational
HM: Isn’t it because a lack of vaccine and the stress it will put on the health system?
WB: Absolutely – it is – but in terms of percentages, it isn’t unlike the flu, without a vaccine. The flu runs at about a 0.1-0.5 per cent case fatality rate. COVID-19 is currently running at 2%, but that’s because we haven’t done enough testing. My guess is it’s going to come down to about 0.5 per cent like the flu. The difference is that no one has ever had it before, and the whole health care system has been overwhelmed, and then the media and internet spread information and with heightened then anxiety and concern escalates. I’m not blaming anyone, but however it’s started, it’s become a global issue, like the flu does, every year, but because the flu is more gradual over a longer time, and has a vaccine, the health care systems cope, and so we don’t hear about it. It’s the overwhelming of the health care system, and the fear of that eventuating, but actually, when you look at the mortality, it’s probably not worse than the flu.

HM: So why have we got military burials in Italy, and New York?
WB: It’s the volume. We don’t know that it’s more fatal than the flu, but it’s attacking and killing the same type of people that the flu kills. When you think about it, who dies when you get the flu? You get the elderly, people with chronic illness, cancer sufferers and the like. That’s what’s happening with COVID-19. Because no one has had the virus before, it’s become overwhelming for health care systems, and so the number of deaths that are occurring are occurring in a small time frame, not over six months. It is a serious health problem, but we will get through this.
HM: The mountain in the US, versus the flattening of the curve here. What’s the right scenario to manage both health and economy?
WB: You could have had a combination. Start with serious isolation and then gradually back off. Social distancing is a good thing, you want to flatten the curve a bit, but you want to try and keep life and the economy rolling. For example, I would’ve tried to keep schools and universities going – but I know there are different views on that – by many people far more experienced than me. I’d keep parks and beaches open with sensible distancing, keep the restaurants open but drop the capacities. Try and Keep life a restricted normal and keep the older, the vulnerable and the cancer patients at home, in virtual lockdown but with strong support of food deliveries and other things to help them. Try and keep people living sensible near-normal lives, recognising that they’re going to get the virus, some will get sick, but most will recover. Only a few will end up in hospital, unfortunately some will die like every year, when we have a bad flu. That’s what we did in 2008 when Australia had H1N1, which was quite a bad flu. Every seven or so years we get a really bad flu, and we all accept that the mortality doubles, but we don’t do anything because we’re used to it. This was a wildfire, because no one else had it. There was no innate immunity whatsoever.
HM: Where do we go from here then in terms of lockdown and balancing health and economy?
WB: What is being contemplated now is: “How do we take our foot off the brake?” Every time we do that, we are going to get a surge of disease two or three weeks later. Then it will be reassessed. My wife and I debate the process from here. She’s a very good researcher and was once an excellent intensive care nurse. We look at the theories – let everyone get it? Lock down until a vaccine? Loosen the lock down and let most people get it and keep the at-risk people at home and help them? I prefer the latter which of course no one has done. The Brits almost did that, the Swedes started to do that, and they’ve all given up, so I guess I’m wrong. Flattening the curve with lock down keeps society functioning, albeit with a huge economic price, and in time I think, a health price through unwanted consequences such as mental health and the effects of delayed medical diagnosis of other diseases and domestic violence.
HM: We will cover the latter shortly, but is there middle ground before the vaccine?
WB: I deal in life and death, and it’s a very difficult decision. I thought the Swedish government was brilliant, but because they had a surge on deaths like you’d expect, they’ve been called inhumane. They made a balanced, rational decision, that was always going to have a surge of deaths. We had 1200 Australians the year before last die of influenza, and no one batted an eyelid. I’m not sure there is a way forward that pleases all. There never is.
HM: Those that are on the front line – are they worried about getting COVID-19, or does it depend on the individual given their age and health? If they’re dealing with these people who have it, why are they not getting infected at higher rates?
WB: The international infections run at 10 per cent of healthcare workers, and some of them will inevitably die. They’re getting it because they didn’t use the right precautions. We know what the precautions are, and people have to take them seriously. Those who die generally have similar risk factors to the general community; the younger ones get exposed to high viral loads so it becomes a massive infection.
HM: Face masks, gloves, disinfectants all essential?
WB: Absolutely. Not touching your face, social distancing, disinfectants as much as you can. They’re all the right things. The masks? It’s probably a good idea, not to protect the shopkeeper, but to protect the customer. If you’re coughing, something might hit them, but the surgical masks don’t work very well to protect you from this virus.
HM: Will we see a rise in mental health issues, depression, anxiety, as a result?
WB: We’re starting to see it, and we’re starting to see an increase in domestic violence both husband against wife, and against children. All of this is going to happen, it’s inevitable, On the other hand, some good things will come out because some families will be camping in the backyard or playing puzzles. We had dinner the other night, one of the kids cooked and we played some board games that we hadn’t played for years, and it was fun. All that is great, but after three or four weeks in our house, everyone’s had enough. I’m the lucky one – I come to work, so I get a break. My wife, the university boy and schoolboy, are doing an amazing job of trying to keep it together.

HM: You don’t seem as worried as I was expecting.
WB: I am concerned, but I’m pragmatic, and in ICU we deal with life and death, and I think I understand the risks. I’d send the kids back to school, I’d get the universities going, and because of that we’re going to have a surge in cases, but that doesn’t mean death. That doesn’t mean an overwhelming of the healthcare system. But we would need to keep a careful eye on those things and be prepared to pull it back if needed. We need to separate cases coming into hospital. The first patient that came into Cabrini had a shower, didn’t need oxygen, was walking around in his isolated room. If he’d have had the flu, he’d have been sent home. We’ve had others since then who got into intensive care, some were sick, and a couple needed tubes and went on ventilators, but a couple weren’t sick and just walked around, had a little bit of oxygen and got better. That’s what you’d expect, ten per cent of people in hospital will end up on a ventilator, and worldwide about 50 per cent of people who are ventilated die. In Australia, we will be much better than that, not because we are naturally better, but we have a better understanding of the illness than the Italians a month ago. We’ve listened and heard what they’ve said and learnt from that.
HM: When you look at the US and how they have dealt with COVID, what do you see?
WB: I saw a total lack of leadership early on. Now that they’ve got going, they are improving. You look at (Andrew) Cuomo, the New York Governor, he’s got it right. He’s co-ordinating and organising for everyone around him, and I think he had a conference this morning that had about eight or nine states all in that area, that are trying to co-ordinate how they back off on their social isolation as a collective. They were slow to react. Our government in terms of co-ordination has been very good. We’ve also been blessed with the fact that we’re separate from everyone else; an island, like New Zealand. We’re a destination, they cut international travel swiftly, which was a great move. They restricted things to community transfer, which is good, but the problem with that is the curve is going to continue at a low level for a long time, because there’ll be no herd immunity unless they start loosening up but then we will need to be prepared for more illness. That will be made easier when testing is more widely available and test results are known quickly.
HM: How long will it take before we have a vaccine?
WB: It depends. You’ve got to test it and make sure it works, you’ve got to also make sure it’s safe. I’m hopeful that we will get one in 12 months or so.
HM: When will we be sitting there talking about the coronavirus as we do the flu?
WB: When we’ve got a vaccine. A year from now we will be living normally again without fear. That’s my guess.
HM: Who came up with 1.5m for social distancing?
WB: All of those distances are made up from bacterial pneumonia and some very old cough studies. I think most of them went less than half a metre, and people just said, “make it a metre and a half for safety!” I don’t think there’s any signs as to whether it should be 1m, 1.5m or 2m. I live near Beach Road, and when I look at the bike riders, none of them are 1.5m apart; a metre at best. I think that’s fine, when you’re out in the fresh air, there’s wind, and they tend not to look at each other as they’re talking. Have you been in a lift?
HM: Last time was round one of the footy.
WB: That was a good weekend! At the hospital, we’ve got incredibly strict social distancing and I got into an elevator and there were six people, and the whole thing was about 9sq m. When I got out of the lift I thought, “well, that’s it, I’ve got to start walking up and down the stairs”. It’s very hard to be dogmatic, and it’s very hard to criticise people. The National Cabinet is making decisions that no Australians have ever been asked to make. We’re going to take a big hit whatever decisions are made. It’s just when you want the hit, and how you want it. I don’t think there’s right and wrong – just the trying to understand what the risks are, and how you find a way through. Someone’s going to criticise you no matter what you do. Really, there’s no magic answer.
HM: COVID-19 – SARS – are there more out there?
WB: Yes – I call it TNV – the next virus. We give blood transfusions in intensive care, but we try very hard not to. People say: “Why are you trying not to?” And I’ll say, “because of TNV – the next virus that we don’t know about”. There will always be another virus, and more importantly, the virus will always mutate in some way, shape or form. For about 40 per cent of people, COVID-19 creates, particularly with children, no symptoms, so you don’t know you’ve got it, or spreading it.
HM: Silent killer.
WB: Yes. Another 40 per cent, give or take, will have very mild symptoms that you might pass off as something else. Then you get to the 20 per cent that have serious symptoms, and they know they’re sick, and then there’s the very small number that end up in hospital and end up dying. It spreads very early, often before you’ve got symptoms. You can get on a plane with it and infect the whole plane, not knowing that you’ve got it, and when you get home, days later, you realise you have it. It doesn’t kill enough, so it’s not a perfect biological weapon. Ebola, which is a perfect killer, kills off everyone in a small area, but can’t get to the next area because there’s no one to carry it there. It gets symptoms early.

HM: Where are we at in terms of testing for COVID-19?
WB: The tests is a swab a swab in the back of the nose and mouth, and that takes 6 hours, or so depending on each lab and the volume being done, the very rapid test geneXpert takes less than an hour … There is also an antibody test, and that can tell you if you’ve had the infection. It may not be positive for two weeks.
HM: Just on the numbers, how many infections are there in Australia at the moment?
WB: We have no accurate numbers because many will have no symptoms and many will not have been tested.
HM: What are the projections on how many we’ll lose to COVID-19?
WB: I don’t know. At the moment, a bit like an army, we’re ready to go, yet we haven’t got anyone to fight yet, because of the government’s policy. That’s really good. We’ve got more capacity if we need to, and we are ready for it. At the moment, thankfully, the government strategies are working. the country has done a great job in trimming the number of deaths as of today – but we mustn’t get excited yet as we still have a long way to go.
HM: When is it projected that our peak infection rate will be?
WB: When this whole thing started six weeks ago, we had a prediction that April 5 was the projected day that the number of patients on ventilators in the country would be greater than the number we had. That was nine days ago, and of course, that didn’t happen. That curve has been flattened a hell of a lot – we’ve hardly got anyone in the state on a ventilator. It’s going to continue for a few months, at least until the end of June. Maybe in May they’ll start trimming one or two things, and then each month they’re going to back off a bit. They’ll have to work out a priority. The peak infection rate originally was early May, then late May, and now we are into June. It is really flattening. The thing people need to think about for a minute, is that most viruses are most active in winter, not summer. We’re coming into winter, so nobody knows how to factor that in.
HM: Why are children generally able to deal with the virus better than adults?
WB: I’m not entirely sure. The actual virus itself is very cunning, and the body’s response to it is very different depending how old you are, and how strong your immune system is. There’s a hell of a lot of unknown about this virus, and that’s why it’s taking people so long to get on top of it. The Brits have learnt that giving really high pressure to the lung is not a good thing, even though that was standard in Italy at the beginning.
HM: Can I ask you a question that has personal motivation – when do you think the footy could get going again and what are the risks?
WB: From a mental health point of view, early to mid-June or worst case, early July. These are very fit guys that aren’t in the high-risk zone. None of those guys are going to die, even if they’ve got it, but perhaps they should stop spitting on the ground and blowing their nose on the ground and sharing water bottles. Football – NRL and AFL are so important to this country – they should start again together – work together and don’t try and rush anything to beat the other. The governments are going to have to ease a few things because again, mental health is so important. I’d be happy to stay at home and watch any footy, even though I’m an Essendon supporter! I thought the decision to play without a crowd was great, and I hoped that it would continue.
HM: We all did, but it felt right to stop ….
WB: I thought playing was the right decision but at the end of the day, we all get caught on the peer pressure and you have your hands tied. That’s the problem with all of us. I’m under the same pressure. We are feeling the pressure of what other countries are doing. On the medical side, anything we can do to help each other, we are doing. I’ve spoken to all the heads of units around the country, and we’re sharing information, asking what you think about that, cross-fertilising ideas. We realise we have to – we are all at risk.
HM: COVID-19 will be with us forever, we’ll just have a vaccine at some point?
WB: Yes – it’ll never go, but we’ll have herd immunity, and calmness. Healthcare workers are learning new things about this virus every week, and how to protect ourselves better. We are learning what works and what doesn’t as treatments, and thankfully the crisis in the USA has led to many trials that will answer questions and help us treat patients better. We are calm and adapting our processes and plans in an expectation of very low mortality – less than last year’s flu. Flattening the curve has allowed time to prepare very well which will allow easing of isolation in a gradual and measured way. Victoria will have all the equipment we need and the capacity to test as required.
HM: Great to hear – thanks so much for your time.
WB: Pleasure Hamish.
MORE NEWS
