Rolling coverage as health bosses appear on first day of hospital inquiry
Follow our rolling coverage of the first day of the parliamentary hearing into the Northern Beaches Hospital, with health and union bosses giving evidence.
Top hospital bosses and union chiefs are today giving evidence at the opening hearing of the parliamentary inquiry into the operation and management of Northern Beaches Hospital.
The $600m public-private hospital run by private operator Healthscope opened in October last year.
The hospital has suffered a catalogue of problems including staff shortages, threats of industrial action, a cancer patient having the wrong part of his bowel removed and a sedated patient falling off the operating table.
Labor Upper House Member and Chairman Greg Donnelly heads Portfolio Committee No. 2 — Health which will see a number of “significant” stakeholders and organisations represented today.
Rolling coverage:
5.01pm Wrap up
Chairman Greg Donnelly wraps up proceedings for the day and thanks those who have appeared to give evidence. The inquiry will continue on September 23. Thanks for joining us today and we hope you have enjoyed the coverage.
4.48pm: Last questions
The respective union bosses use their last few minutes to give an update on progress.
Mr Ravlich said that survey results show it is better than what it was back in October. He adds that work still needs to be done.
Mr Hayes adds that there is still an “adversarial relationship” with Healthscope and describes it as “working against a brick wall”.
Mr Holmes tells the inquiry that “running of public health should be under the control of the public system”.
He adds: “We see what happens when you’ve got two different lots of staff and management and frankly it is not pretty…”
Mr Dalton concludes by saying there are still outstanding matters. He adds that staff are disappointed that their working experiences are still short of what they experienced when employed by NSW Health.
4.55pm:
Mr Hayes talks about increase in “pressure injuries of newly discharged patients”.
He tells the inquiry these injuries occur when rolling a patient who has been bedridden for some time to relieve pressure.
“Pressure injuries only really occur when there is a lack of staff,” he said.
4.45pm:
Mr Holmes said his members felt “professionally liable” when they went to work.
He said members went to work and were concerned on every shift that their registration was at risk as a result of working in an environment where there were not enough staff to match needs of patients.
They also said they were working with people who did not have skill level required to be looking after patients.
“They considered themselves professionally liable but powerless to make effective change,” he said. “They felt they had to go to work and do the very best they could but there were things beyond their capacity and that created a highly stressful environment.”
4.39pm: Policy lacking
Mr Holmes was asked whether the opening was rushed. He said there was little or no orientation for new staff and a dearth of policies and procedures as far as staff are concerned.
He said he visited three or four months after opening and staff told him they still didn’t know about policies and procedures.
4.31pm:
Mr Holmes said midwives had expressed concerns regarding increased intervention procedures.
He said concerns had been raised that it had gone from a “midwifery model of care to an obstetric model of care”. He added: “which means that the obstetricians are making the decision about things like discharge and care.”
He said members also believe that they are seeing an increase in the caesarean rate and intervention.

4.25pm:
Walt Secord asks if there are enough workers to run the hospital safely?
Hayes: I think clearly support staff that we represent are indicating that there are not enough staff.
4.20pm:
Mr Hayes says that IT issues have been causing his members real problems.
Royal North Shore can’t get info from Northern Beaches Hospital, he said.
“It is a slow process to share information and a lot of opportunity is lost,” he said.
He said NBH is still using a DOS computer system which was utilised back in the 1980s.
Not compatible and not fit for use in 2019, he adds.
4.15pm:
Mr Holmes said the union’s concerns were always based on poor previous experience with public-private health systems.
“They can’t be trivialised as teething problems,” he says of initial problems.
The extent of the crisis on opening was “profound and significant,” he adds.
He says the issues on opening are the result of either “brazen untruths, sheer incompetence or a cocktail or both”.
“It is impossible to accept they didn’t know the poor state of staffing from day one.”

4.09pm: More unions leaders are up:
They are: Brett Holmes from NSW Nurses and Midwives Association and Branch Secretary of Australian Nursing and Midwifery Federation;
Mr Dennis Ravlich Manager, Member Industrial Services Team, NSW Nurses
and Midwives Association; Kieran Dalton Australian Nursing and Midwifery
Federation Branch Organiser, Northern Beaches Hospital; Gerard Hayes Secretary, Health Services Union NSW and Brendan Roberts Organiser, Health Services Union NSW.
4.05pm: Emergency doctors doing a great job
Dr Sara: The issue isn’t in ED, it’s what’s happening behind that. There’s not enough staff or policies or procedures. Emergency department doctors are doing a great job and the best they can.
4:04pm: Bundy system
Dr Sara: Junior doctors told they would have to tap on and off when they came and left. It doesn’t happen anywhere else. They will never ever be working less than scheduled, but they are only getting paid for eight hours. He says it’s an actual “slap” to doctors to ask them to bundy on and off.
Ms Maclaren-Jones says could it be used to build up evidence that they are building up overtime?
That’s not how it was presented by management, says Dr Sara.

4pm: Royal North Shore Hospital:
Dr Joseph: There’s no doubt that services (at Northern Beaches Hospital) have improved over the past couple of months but it is clear that a certain number of patients do not have confidence, along with some GPs
He says RNSH is still receiving stroke and interventional cardiology. The Northern Beaches Hospital does not have the confidence in the community. One lady took a $100 taxi from Narrabeen to RNSH because she didn’t have confidence.
3.55pm: Pathology: Pathology provider ‘less than optimum’
Dr Sara: Pathology system is less than optimum and the pathology provider is less than optimum. They cannot do proper reports and they still mislay specimens, he says. He then claims that’s what happened when the wrong part of a patient’s colon was removed.
He says the pathology system is set up for a private hospital which is light and easy, not very unwell public patients.
He says the pathology lab clearly cannot do what it is required to do. It’s more suited to “office practice” than public hospital, Dr Sara says.
3.48pm: Six out of eight have failed
Ms Faehrmann asks “do you think the Government will have to rescue or buy back the hospital?”
Dr Sara: Six out of eight (public-private) have failed. The likelihood is that it will fail.
3.42pm: Taxpayer funded doctors are treating private patients:
Dr Sara: Many junior doctors see private patients. It is now part of their duty. It’s changed from the original model.
3.41pm:Are private patients being looked after by NSW Health employees?
Dr Sara: Public and private patients are mixed. If someone is very unwell and needs something right now they are obligated to save their life. It was to be quite separate but it has become very blurred. Junior medical officers even though they’re not meant to be looking after private patients they are now. The difficulty comes back to workload.

3.36pm: Ongoing issues
Dr Sara continues to list what he says are ongoing issues.
He says accreditation is not in order and there’s question marks on policies, procedures, etc.
He also agrees that it is indeed a two-tier system.
“It is a Level 5 for public and Level 6 for private.
“It is a two-tier system.”
3.33pm: Bundy system
In the last few weeks management wanted doctors to bundy on and off, Dr Sara says adding it would be the only place in Australia where that happens.
“We went in to bat for the young doctors,” Dr Sara said.
3.31pm: Surgery priority
Dr Sara: To begin with elective surgery lists would start on time every morning, taking priority over emergency patients waiting from the night before.
Priority has changed since then and “it is on the mend”. I suspect that aspect of the culture has changed.
3.26pm: ‘19 hour locum shifts’
“There’s a lot more work to do”.
When the hospital opened there were many issues including no Panadol in the Emergency Department. Have things improved, Mr Secord asks.
Dr Sara: Yes, but it took many months to occur. All the issues the young doctors identified have been addressed apart from adequate staffing, IT system and proper policies and processes, and too many locums. A few weeks ago surgical locums were starting at 5am or 6am and working until midnight. That was sorted.
3.19pm: Bite the bullet
NSW Government should bite the bullet and buy it back now says Dr Joseph.
3.17pm: ‘Hospital will fail’
Dr Sara: My suspicion is that Northern Beaches Hospital will fail in due course. It’s been very poor to date. He says he can’t say whether it will be a failure long-term?
“We have to get rid of the Triple P model once and for all,” he says.
3.13pm: On policy and procedures:
Dr Sara: Six weeks ago I met with staff specialists and they are not happy. Not happy with clinical policies. They’ve only done six in a year. We need proper policies and processes.

3.12pm: “Public Private cannot work”
Dr Sara: Public-private can never work. A triple P (Public Private Partnership) hospital in Victoria is being brought back into public care. The issue was about public safety. Six out of eight triple P models in Australia have failed, he says.
3.08pm: “Disaster narrowly avoided”
Dr Sara: It’s hard to fathom how a hospital can be set up without advice from senior doctors. Everything they warned about came to fruition. On opening disaster was only narrowing avoided. It was a distressing time for junior doctors, it was a nightmare.
We don’t deny major improvements have been made but it’s still understaffed, proper policies and systems are still not in place and patients are still falling through service gaps.
3.03pm: Union bosses are next up
Dr Tony Sara President, Australian Salaried Medical Officers Federation of NSW
Dr Anthony Joseph FACEM Senior Staff Specialist, Emergency Department and Director of Trauma, Royal North Shore Hospital and NSW State Councillor, Australian Salaried Medical Officers Federation of NSW
2.55pm: Phew, it’s time for tea. Time for people to cool down.
2.52pm: Pointing fingers
National Upper House Member Wes Fang is told off for pointing his finger at the audience. Mr Donnelly loses temper, as Mr Thomas puts his head in his hands.

2.50pm:
Liberal MLC Shayne Mallard gives the community representatives a grilling, as Mr Secord asks him to apologise.
2.40pm: ‘Mona Vale is my passion’.
Mr Thomas, in response to questions about his ambitions said: “Mona Vale Hospital is my passion.
“I believe fundamentally the delivery of hospital services on the northern beaches is sub-standard.
“I think the new hospital should be a Level 6. We have said we would be be happy with a Level 3 hospital at Mona Vale. We need to meet the growing population.”
2.35pm: GetUp claims:
Mr Thomas denied he had associations with any political party or GetUp.
Mr Thomas said he was not politically aligned.
He said: “I have not been involved or aligned to a political party”.
“It is a community issue, it is nothing but a community issue,” he says.
“Order! Order!”
Mr Donnelly calls for order and Ms Faehrmann says we should not badger witnesses, as Mr Thomas is quizzed on his political background.
He was asked questions about his views on the council amalgamation.
2.30pm:
On the level of care provided at the hospital Mr Thomas said: We are continually told it is Level 5, but we hear feedback from doctors and nurses to say there’s a whole load of services that are not Level 5.
They are providing some services to a Level 6 for private patients.
He said if you walk around the hospital it integrates public and private and it might have sounded like a good idea at a time. It should have been a co-located private building, says Mr Thomas.

2.27pm: Mona Vale Hospital Urgent Care Centre
Health Minister, Brad Hazzard has said the UCC would meet the requirements for a Level 1 Emergency Department.
But Mr Thomas says the reality is it’s an Urgent Care Centre.
It’s the “basics of basics” and we don’t believe it complies with a Level 1 Emergency Department. “People want their emergency department back,” he says.
2.25pm: Maternity
Transparency is “less than ideal” says Ms Mooney.
“We have had to push for every single meeting we ever had.
“We are very unhappy with every level of engagement we ever had.”
2.20pm: Mr Thomas, the head of Save Mona Vale Hospital Action Group, said it’s not about comparing with what we had, “it’s about what we have now and what we should have now”.
He said the peninsula’s north needs more.
The model needs to be tweaked and changed.
The population demands says so.

2.15pm: Location of hospital, travel time increases:
Mr Thomas says the ambulance union talks about increase of travel times.
It says it has “significantly increased for member of the community”.
Patients now need to get themselves to Mona Vale, you can get a bus from there. He says it’s a substantial amount of time to get there from Mona Vale north actually.
He adds the Wakehurst Parkway regularly floods or has bushfires.
“We had a time recently that every single access road apart from McCarr Creek’s Rd was flooded,” he said.
2.05pm: Agency nurses don’t build a relationship with the patient, says Mr Thomas. He said he has been hearing there are significant agency numbers.
Mr Thomas said he was told that someone was taken by ambulance to NBH with a heart attack but an agency nurse got the quantities of drug wrong.
He asked to be transferred, and eventually was but transferred without notes.
Mr Thomas says a lot of GPs are advising their patients to go to Royal North Shore.
He also claims senior people from Northern Sydney Local Health District are also doing the same.
He continues to say a lot of GPs are advising their patients to go to Royal North Shore.
He also claims senior people from Northern Sydney Local Health District are also doing the same.

2pm: Mr Walker asks if the cladding used on the hospital is safe. He says he’s put in a GIPA, but not got any answers.
1.56pm: Mr Thomas says the vast majority of patients are from the beaches catchment, but Frenchs Forest is not the northern beaches, it is away from the beaches’ strip.
Many patients are now coming from Chatswood, Turramurra and St Ives, but the hospital numbers are similar.
1.53pm:
Ms Mooney says midwives have anecdotally revealed that there is more intervention during births at Northern Beaches Hospital, than in the previous hospitals.
She’s calling for statistics to be revealed sooner than next year to see what the true picture is.

1.48pm: Maternity concerns
In her opening statement Ms Mooney said her main concern is that Healthscope has “zero experience” in running maternity facilities and services.
She also says there has been a lack of meaningful engagement with community representatives. Her group is the only maternity group on the beaches she said, adding that she was concerned that they weren’t spoken to.
She also said the number of midwives is still inadequate.
1:43pm: Fire safety concerns
In his opening statement, Mr Walker says he has concerns over cladding and fire safety at the hospital and calls on the inquiry to investigate.
1.39pm: Patient quality
Mr Thomas says issues have been raised to him on a daily basis.
“I’ve got to say to you I’ve stopped going to my local pharmacy and I can’t get out because I get listed all the issues,” he said.
He said the community needs the hospital to work. He said the “co-location” concept could work but only with a private and public hospital next to each other. It can’t work with amalgamated services, he adds.
1.33pm: Back underway:
We are back underway for the afternoon session. Giving evidence first will be Parry Thomas, chairman of the Save Mona Vale Hospital Action Group, Phillip Walker, Honorary Secretary of Friends of Mona Vale Hospital and Mrs Helena Mooney, co-founder of Friends of Northern Beaches Maternity Services
1.20pm: More questions on transfer of patients
Dr Woods says it is appropriate to transfer those with particular needs, especially children who need to be operated on and trauma cases, as Northern Beaches Hospital is not a trauma hospital.
1.18pm: Staff numbers
The next question is regarding staff numbers. Is the lack of permanent full-time staff a cost-saving strategy?
Mr Royle says the hospital has nearly 1800 staff, 43 per cent are full-time, 28 per cent are part-time, 29 per cent are casual.
He adds it is not uncommon for public or private hospital to use casuals.
He says they only have 34 full-time equivalent vacancies adding that they have recruited strongly in recent times.

1.12pm:
Waiting times significantly worse than Manly or Mona Vale Hospital?
Dr Woods says IT challenges and the data were uncomplimentary and staff were saying it was not a true representation of what they were seeing.
They did a review and staff were right that they were delivering timely care.
1pm: Back to beds - again.
Ms Hurst apologises about coming back to bed numbers again.
Dr Woods says it’s based on services, not bed numbers.
He says there are “ebbs and flows on the number of beds allocated to particular specialties”. He says at the moment they have a higher number of patients with respiratory issues, but later in the year there will have a higher number of babies being born
12.55pm: Level 5 hospital
Dr Woods says Northern Beaches Hospital does have the capability to provide services above a Level 5 hospital.
Cardiothoracic and neuro surgery for example is available to private patients.
Mr Gameren says NSW Health is aware that we are providing those services to private patients.
12.50pm:
Patients pressured to use private health insurance:
Mr Spillane denies that patients are being pressured to go into the private system.
12.45pm:
Heart attacks: Dr Woods says paramedics are asked to take those that appear to be having a heart attack to Royal North Shore.

12.40pm: Back to beds
Mr Royle says 291 public acute beds available and at times used.
There are a 195 private beds. There were 279 in Manly and Mona Vale, but some of those were rehab beds or non-acute beds.
Secord says: “So just 12 more beds at the new hospital?”
Later, Mr Spillane says the hospital is licensed by NSW Health for 486 beds. 439 are overnight beds, 41 are ED treatment spaces and six are paediatric short stay beds.
As of last night there were 363 patients in beds, 187 public and 176 private.
•12.35pm: On the issue of senior staffing, Mr Secord asks if there are any more vacancies.
Dr Woods responds saying they need more dermatologists.
•12.30pm:
Orthopaedics sector is lucrative says Mr Secord, compared with complex medical issues.
“It has been put to me by doctors that you are doing things like orthopaedics and sending more complex procedures to Royal North Shore Hospital?”, he says.
Dr Woods says a small number of complex patients are transferred to Royal North Shore.
And the committee reveals that young doctors were doing 110 hour weeks just after the opening.
Dr Woods says it was “excessive” in some areas at the start.

•12.25pm: Sentinel events:
A sentinel event is an unexpected death, or near miss.
When asked how many sentinel events have occurred at the hospital:
“I am aware of two which have been subjected to the Root Cause Analysis,” says Dr Woods.
Mr Secord says there are 15 to 18 sentinel events in the state a year.
But Dr Woods says there would be more than that.
• 12.20pm: There has been a bit of a furore over the breakfast differences between public and private. But Mr Gameren said public patients can request hot breakfast as well.
• 12.16pm: Was it ready to open?
When asked was Northern Beaches Hospital ready to be opened?
Mr Gameren says it’s a matter for debate, but the hospital’s leadership believed it was.
•12.15pm: 17 patients spent 24 hours in Emergency leading to financial penalties:
Mr Secord asks: Did you put forward that you should not get the full payment over the past months?
Mr Gameren says they did suffer financial penalties.
In November they were 17 instances where patients spent 24 hours in ED. The standard is that no more than four hours should be spent in ED before a patient is transferred to another ward.
He says they were cared for, they were in a bay but they were not moved into a ward bed or discharged in that time.
•12.12pm: Next up: Richard Royle Interim Chief Executive Officer, Northern Beaches Hospital, Dr Simon Woods Interim Medical Director, Northern Beaches Hospital, Stephen Gameren State Manager- Hospitals (NSW/ACT) and Healthscope Mr Andrew Spillane Director of Finance, Northern Beaches Hospital
•12.10pm: Financial penalties:
They are working very hard to provide a stellar service, says Ms Willcox.
Financial penalties have been applied in previous months, according to chairman Mr Donnelly.
Ms Willcox says Healthscope reviews the data and they apply the abatements to themselves.
•12.05pm: Ms Maclaren-Jones asks about Save Mona Vale Hospital’s submission which says Northern Beaches Hospital does not meet community needs going forward.
Ms Willcox responds by saying the hospital is supported by the new Brookvale Community Health Centre which provides many services, also refurbished community centres at Seaforth and Mona Vale.
There’s also a palliative care unit at Mona Vale.

•12pm: On the issue of patients being taken to Royal North Shore Hospital:
Liberal Upper House Member Natasha Maclaren-Jones asks why patients are transferred to Royal North Shore Hospital.
Ms Willcox says 20 per cent of ambulances would take patients to Royal North Shore before the new hospital opened, now it’s believed to be 11 per cent, allowing for more northern beaches residents to be treated closer to home.
• 11.55am: Now a question on maternity services.
Why have submission targets and thresholds of maternity services been redacted from the Project Deed, asks Ms Faehrmann?
Ms Willcox says she will take that question on notice.
She then goes onto ask what is an annual cap in the Project Deed.
Does it mean the private operator can’t get to see more public patients if it hits its annual limit?
Dr Lyons explains how, like all public hospitals, there is a fixed budget.
He says there’s a finite budget and increasing demand in healthcare which is something all public hospitals have to manage.

•11.52am: Bed numbers
Ms Faehrmann says when it comes down to it, beds and waiting times and services provided are “unsatisfactory” according to the submissions.
Dr Lyons says we should not make direct comparisons. Northern Beaches Hospital is providing a higher level of service and you can’t just look at beds and counting beds, you need to look at length of stay and complexity of patients before we make any comparisons.
“Don’t just look at bed numbers,” he says.
•11.45am: Is the State Government paying less for Northern Beaches Hospital compared with Manly and Mona Vale?
Dr Lyons said you cannot compare make a direct comparison.
He says more is being provided for NBH but it is a different level of service it is not like for like.
•11.42am: Do patients have to pay for pathology tests now?
Ms Faehrmann says submissions reveal that patients are having to pay for pathology tests that they used to get for free and that there are no longer public neurology or cardiology services available.
Ms Willcox says there are a raft of outpatient clinics
•11.40am: Questions about the contract (project deed)
Greens Upper House Member and Deputy Chairman Cate Faehrmann asks whether Healthscope provides for public patients services they could have for free in Manly and Mona Vale hospitals?
Dr Lyons responds that the project deed was not formed that way, there was a certain number of clinics that would be purchased but there was a recognition they were moving from one model of care to another model of care.
Ms Faehrmann says was it one that public patients having to pay more for services and more out of pocket costs?
Dr Lyons denies that is the case.
•11.30am: Row over public beds
Ms Hurst says there appears to be only 300 public beds at Northern Beaches Hospital, but there were 350 public beds at Manly and Mona Vale hospitals combined.
Ms Willcox says to her knowledge she thinks there is a 60/40 private to public split, but you can’t compare the numbers.
“We are purchasing the public activity,” she says.
Dr Lyons says public beds is a matter for Healthscope.
“I can’t tell you what they are”, he says.
“But you are paying the bills”, Mr Secord cries out.
“You don’t know how many beds you are paying for?”
Dr Lyons says NSW Health is contracting for a level of service and the number of beds “may change on a day-to-day basis”.
“We actually purchase for service,” says Mr Lyons

•11.20am:
Animal Justice Party Upper House Member Emma Hurst asks why was the Northern Beaches Hospital built as a PPP model rather than public?
She asks why was a public private model better for this specific community?
Dr Lyons responds saying that non-government or private operators provide many services throughout our health system.
There are many examples of private operators providing public services and other examples of PPP’s across the state.
She then asks why the compliance and inspections checks did they not identify the lack of basic stock IV fluids and syringes before the opening.
Dr Lyons says the issue with stock was procurement in the supply chain and that there was stock on opening.
•11.15am: On the high number of senior staff departures: Mr Secord asks about major staff departures since opening, including the CEO, head of nursing, medical director, head of anaesthetics. Ms Willcox says she knows of no other senior staff departures.
•11.10am: Mr Secord asks why the hospital 50 fewer beds than what the contract originally asks?
He pointed to Ms Wilcox’s submission which says there’s 423 beds. “Why does the hospital have 50 fewer beds than the original contract?” Mr Secord asks.
Ms Willcox says there’s currently 350 beds open as they progressively bring beds online and recruit staff. She says there’s an ability to open 488 capacity, if required.
Why only 350 beds, says Mr Secord?
Dr Lyons says the project deed provided for at least 423 with a minimum of 173 private patient-designated beds.
• 11.05am: Was the hospital ready to open?
Ms Willcox: Independent verifier gave us a certificate of readiness.
Our job was to move Manly and Mona Vale staff across and get everything in place.
Healthscope was responsible for the rest.

•11am: Mr Secord asks what Healthscope has to do to have the State Government take action or reduce state funding.
“Will you continue to pay them for 20 years but not check patient care?”, he asks.
Ms Willcox says there’s a suite of abatement provisions, there will be a reduction in the payment where certain things are not met.
Those “provisions have been applied in previous months”, she says.
“But we want to build a strong and positive relationship with Healthscope working through the issues collaboratively”.
•10:50am: Mr Secord asks did NSW Health continue paying Healthscope its monthly service payments “regardless, despite complaints and problems at the hospital”.
Dr Lyons says yes. He says NSW Health took the view that for the “operation of this hospital to be a success” it needed to support the operator.
He said it would not be in the operator’s or patients’ best interests “for us to proceed down a path of going to contractual interests straight up”.
Mr Walt says: “But you are paying the bills for this?”
Dr Lyons: “Yes we are but we want a positive partnership”, adding he thinks NSW Health is “getting good value”.
•10.40am: Mop-gate:
Mr Secord asks whether it was still the case that there was just one mop in one bucket for every two wards in the hospital and that it took nine weeks to get more mops for the hospital.
Dr Lyons says Healthscope is responsible for the operation of the hospital.
•10.37am: Labor committee member Walt Secord asks whether there’s a two tier system in the hospital after quoting from the Health Services Union’s submission to the inquiry. Willcox says there is not.
Mr Secord asks why then are staff told to provide hot breakfasts to private and cold to public?
“I’m not aware of such stark differences”, Ms Willcox says. “I would be concerned if there were major differences between public and private patients”.
Mr Secord says there seems to be a “healthcare apartheid on the northern beaches”.
•10.32am: Deborah Willcox says NSW Health meets frequently and regularly with Healthscope executives and there’s a performance framework to measure safety and quality issues.
She said that the two have day-to-day contact and formal meetings every day.
In answer to Labor Upper House Member Walt Secord’s question of whether patient care had improved since opening she says yes.
When asked about issues with supplies and services she said NSW Health “worked quickly to support Healthscope and provide all the resources at our disposal”.

•10.25am: Ms Deborah Willcox says the independent verifier was satisfied Healthscope was ready to open and the hospital was fully accredited 10 days after opening.
While a number of issues emerged after the opening, Healthscope was responsible for the operation and NSW Health acted swiftly to help, she said.
She added that patient flow was identified as an early issue. NSW Health gave advice and support.
“It’s a long-term partnership,” she said of the link between NSW Health and Healthscope.
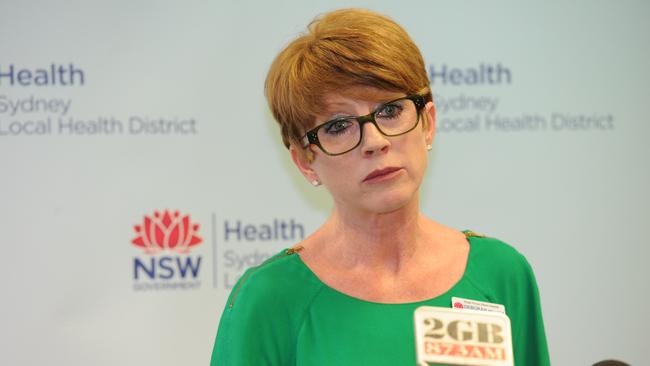
•10.17am: Deborah Willcox Chief Executive, Northern Sydney Local Health District, is also now giving evidence alongside Dr Lyons.
“Planning was meticulous,” she tells the inquiry. “The new hospital was a very large undertaking and many years in the planning.
“What we have now is far more than what was before.”

•10.15am: Dr Nigel Lyons, Deputy Secretary, Health System Strategy and Planning at NSW Ministry of Health is first up.
He acknowledges the “heartfelt and personal submissions” from individual and local organisations and “their passion for their local hospital”.
He also praises the staff for the exemplary efforts and hard work.

•10:07am: Labor Upper House Member and Chairman Greg Donnelly opens proceedings: The inquiry will look at the management and operation of the hospital, public-private merits in healthcare and the impact on Mona Vale Hospital. He says there’s significant interest of people from the peninsula about the inquiry.
• 9:40am: Witnesses will include Dr Nigel Lyons Deputy Secretary, Health System Strategy and Planning, from the NSW Ministry of Health and Deborah Willcox Chief Executive, Northern Sydney Local Health District and a number of hospital executives.
In the afternoon leaders from several unions including the Australian Salaried Medical Officers Federation of NSW, NSW Nurses and Midwives’, Member Industrial Services Team and Health Services Union NSW will answer questions.
Others that will appear include campaigners for Mona Vale Hospital Friends of Northern Beaches Maternity Services.
IN OTHER NEWS


