Immune cells engineered to destroy cancer offers hope to leukaemia sufferers
A NEW trial which uses the body’s own immune system to identify and kill cancer cells is offering adults and children with leukaemia new hope. This treatment will be used in favour of chemotherapy, which 11-year-old Mackenzie Isedale underwent.

NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
- Why Aussies are heading to Mexico for brain cancer treatment
- First-time mum gives birth to her ‘little miracle’ at age 50
TWO years after Mackenzie Isedale began her gruelling journey to beat leukaemia, the 11-year-old last week rang the bell on her last chemotherapy treatment.
The toxic medication had left her bald, sick with painful ulcers, incapacitated for months and unable to walk. For her mother Errin it was a nightmare to watch her previously bubbly girl become so debilitated in pursuit of a cure.
“It was heartbreaking, she went through a stage when she couldn’t walk for three months and to see your bouncy nine-year-old who loved gymnastics to be stuck in a wheelchair was awful,” Mrs Isedale, from the small town of Welby in the Southern Highlands, said.
“It was hard to explain to her she had to get sicker to get better.”

But in a potential ‘game changing’ trial to start soon out of the Westmead Institute of Medical Research, other children and adults may be saved from having to endure such excruciating and exhausting chemotherapy treatment for Acute Lymphoblastic Leukaemia (ALL).
Rather than rounds of toxic chemotherapy drugs designed to kill cancer cells, scientists will use the body’s own immune cells, called T cells, re-engineering them to recognise and destroy cancer cells before reintroducing them into the body.
Paediatric oncologist Dr Luciano Dalla-Pozza said the trial, which will recruit patients next month, had the potential to lift survival rates from the current 80 per cent to near 100 per cent.
“The cure rate with chemotherapy at the moment is 80 per cent, but 20 per cent will need a bone-marrow transplant and only half those will respond. The CAR-T cells will be trialled on the remaining 10 per cent,” he said.
“There’s a clear prospect a lot more will be cured. That small group of children we fail, immunotherapy seems to have an astonishing effect and we hope that translates to a cure.”
The treatment cured Emily Whitehead, a 12-year-old from the US who had failed all other treatments.
Diagnosed with ALL at age five, she relapsed twice despite extensive rounds of chemotherapy. A bone-marrow transplant fell through at the last minute and in desperation, her parents enrolled her in a phase 1 CAR-T cell trial.
At age seven, Emily became the first child to receive the therapy at the Children’s Hospital of Philadelphia.
Her T cells were extracted from her blood, “reprogrammed” and multiplied in the lab to target and combat her cancer. This army of “hunter” T-cells was then infused back into her body.
She is now five years cancer free and her T cells are still working to identify any new cancer cells.
“That single success, when none was anticipated, it was pie in the sky stuff, but to see that happen and then reinforced with repeated success is really promising,” Dr Dalla-Pozza said.
Early results from clinical trials have reported 93 per cent of paediatric patients with relapsed ALL have achieved remission.
“T cells help protect us from developing cancer but cancer cells have developed a way around detection, the T cells don’t see the cancer. We put a new kind of receptor, like a key in a lock mechanism, into the T cell so it can see the tumour cells,” Dr Ken Micklethwaite, group leader for CAR-T cells research at Westmead Institute of Medical Research, said.
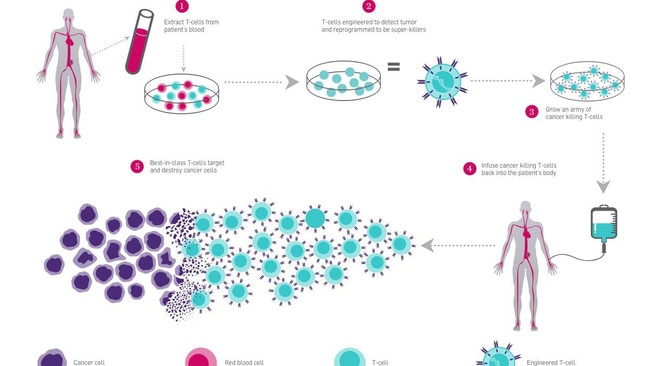
The ‘key’ is created with an antibody that recognises the tumour and is combined with a new protein whose gene is then introduced to the patient’s T cell, grown in the lab and infused back into the patient.
“Hopefully this will replace chemotherapy. I see a future where a patient presents, has cells collected, has some chemo to debunk the tumour and after one month given the CAR T cells and that is likely the only treatment they will need,” Dr Micklethwaite said.
Mackenzie Isedale, who is an ambassador for the Children’s Cancer Institute’s “Endure for a Cure” campaign, is now well but will need monthly blood tests to check for relapses.
“It would be wonderful for the kids that are diagnosed now that could do immunotherapy rather than putting all these toxic chemicals into the body,” Mrs Isedale said.
* Follow Jane Hansen on Twitter @janehansen2000 or email jane.hansen@news.com.au


