What Covid does to your body: Inside an ICU treating coronavirus patients
Intensive care specialist Dr Mark Nicholls reveals exactly what happens as Covid ravages its way through the human body — and how his team fights back.
NSW Coronavirus News
Don't miss out on the headlines from NSW Coronavirus News. Followed categories will be added to My News.
Dr Mark Nicholls is an intensive care specialist and vice president of the Australian and New Zealand Intensive Care Society. For the past 18 months, he and his colleagues have been caring for those Covid cases that end up in intensive care.
As an intensive care specialist, Sydney-based Dr Nicholls has one aim: to get patients out of intensive care alive.
“It is very hard for us to give up. We will do our absolute best to get someone home. We are committed to that outcome and we will do everything we can to get that person to survive and get home,” he said.
Here he gives an insight into what the virus does to your body once it gets into your lungs and what our medicos do to try to save you.
This is how it starts.
You breathe the virus into your nose or mouth, or pick it up from a surface and transfer it to your nose, or mouth, by touching your face after coming into contact with an infected person.
“The virus comes in from the nose and the mouth where there are receptors on the cells called ACE2 receptors. There are a lot of them in the nose and the mouth and that is the part, the spiky part of the virus can attach to. Once it attaches to those cells, the virus then moves into the cells and it uses the internal mechanics of the cells to reproduce itself,” Dr Nicholls said.
As the virus multiplies, it works its way down the respiratory system.
“The virus starts progressing down into the lower part of the respiratory system (where) you have the alveoli sacs, the part of the respiratory system where oxygen passes into your body and carbon dioxide passes out of your body.”

The membrane of these sacs contain a high number of cells with ACE2 receptors which the virus attaches to, causing inflammation.
“You get this inflammatory reaction and then these sacs fill with fluid and then you have impairment with oxygen going in and carbon dioxide going out,” Dr Nicholls said.
“Because there is fluid in the lungs and this cellular reaction in the lungs, the lungs get stiff and you need more effort to breathe.”
At this point, getting air into the blood and carbon dioxide out is becoming harder, so the patient starts to feel breathless.
In hospital oxygen is given and patients have early access to intervention drugs that will help.
“Once in hospital we provide patients with nasal prong oxygen, we keep monitoring their oxygen requirements to see how they are working from a breathing perspective and we measure their oxygen saturation,” Dr Nicholls said.
“You can still deteriorate quickly despite coming to hospital. We have patients who come in to hospital early and are on a small amount of oxygen and within a short period of time they progress to needing to go to ICU.
“So you can imagine if patients are staying at home and getting sicker, by the time they come into hospital they could be very sick. One (drug) we use is dexamethasone, there is evidence it improves survival.
“We use it as people start to use supplementary oxygen. And depending on severity, we also start using Remdesivir, an antiviral that impedes the virus’s RNA production in the cells.”

Sometimes the body’s own immune system overreacts with what is called a cytokine storm.
“The cytokine storm is when an overactive inflammatory state is causing injury. You have an inflammatory response to the virus, you hope the response is proportionate to the virus, but that it clears the virus and people recover. But in a cytokine storm, what happens is the immune system is so overactive and maladaptive it is turning back and causing injury, it is an excess inflammatory response that is counter-productive,” Di Nicholls explained.
“This is why we use a drug called Tocilizumab, or more recently Baricitinib. These drugs help with the cytokine storm.”
If the patient is unable to maintain oxygen saturation in their blood at 92 per cent, on nasal prong oxygen flowing at six litres per minute, the protocol is to move the patient to ICU.
“When we move a patient into intensive care, they are already moving to a point where they need high flow oxygen. You can deliver it at 40-50 litres a minute flow and with that high oxygen requirements. Air is 21 per cent but we can run this oxygen up to 80, 90 or 100 per cent.
“With half the patients, when you have done that combination of drugs and the high flow oxygen, they stabilise, are reasonably comfortable and after a few days start to improve.”

Then there are the patients who deteriorate.
“If they get to a point where they are having increased work breathing because the lungs are stiff and they are starting to struggle, we can try something called non-invasive ventilation, which is a mask to the face, attached to a machine that provides positive air pressure and oxygen. It gives some assistance, with higher pressure when you breathe in and a lower pressure when you breathe out,” Dr Nicholls said.
If the patient continues to deteriorate, the decision is made to intubate and ventilate. The patient is given a sedative anaesthetic. They are often paralysed to decrease oxygen requirements and synchronise the patient with the ventilator.
“For some patients, we intubate because the lungs are too stiff for the non-invasive ventilation to work. Intubation is where a tube is inserted into the throat and the trachea (windpipe). The tube has a cuff on the end which is inflated for a seal. The tube is then connected to a ventilator. A ventilator is a device that supports or takes over the breathing process, pumping air into the lungs.
“When ventilated, we prone most patients. We physically turn them over, so rather than have them on their back, we turn them on to their abdomen. That changes the physiology of the lungs, changes the blood flow in the lungs, and actually improves oxygenation.
“We turn them over during the course of the day and then leave them until the next morning and turn them back on their back. You have improved oxygenation, but then you prone them again in the evening and un-prone them the next day.
“When we see a sustained improvement we start weaning (the patient) off the sedation and seeing if we can extubate (take the breathing tube out).”


Intensive care is an incredibly controlled environment, but things can still go wrong with Covid.
“For cardiac arrest to suddenly occur is unusual, but that is not to say it can’t (happen), Dr Nicholls said.
“With Covid, it has a tendency to cause clots in the veins and the legs, so (the patient) can get pulmonary embolism and that can cause a cardiac arrest.”
Sometimes, as is the case with 949 Australians to date, no amount of intervention can cure the curse of Covid.
“You go to the ventilator, you’ve done the proning, but things worsen and it comes to the point where you can’t ventilate the person no matter what you do.
“You can’t oxygenate, you can’t remove the carbon dioxide, or you have septic shock or sepsis and you can’t support the blood pressure,” Dr Nicholls said.
“We will do everything we can to help that person get home, but there are limits to what the equipment we’ve got can do. In some circumstances, it’s not survivable.”
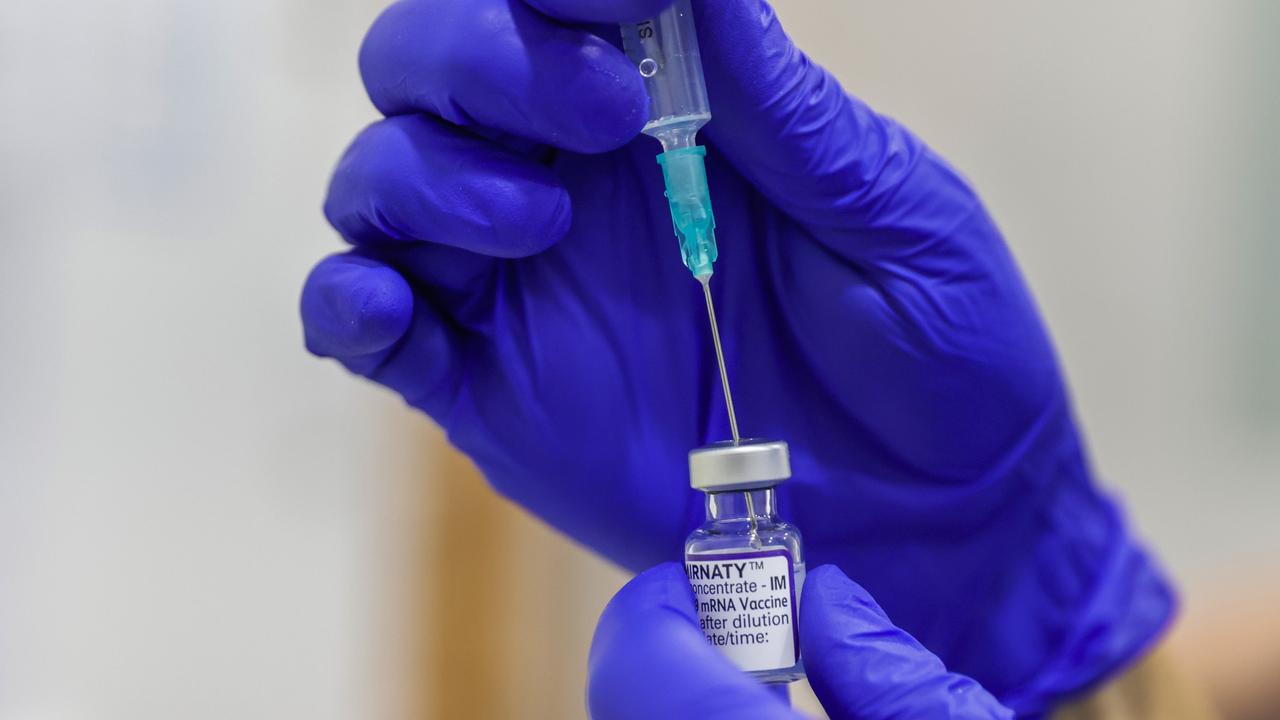
A growing body of evidence is proving vaccines can keep Covid patients out of hospital.
“Recent evidence for the Delta variant of Covid is that the AstraZeneca and Pfizer vaccines are 90 per cent protective of hospitalisation, ICU admission and death. How can you not be vaccinated with that degree of protection?” Dr Nicholls said.
More Coverage
Originally published as What Covid does to your body: Inside an ICU treating coronavirus patients