YOU’VE probably seen a 3D printer.
They were all the rage a few years ago, with news bulletins of 3D printed guns that actually shot bullets and playable musical instruments working viewers into frenzied discussions of what next and to kids asking for cheap versions for Christmas so they could make real-life copies of their Pokemon doodles.
But at The University of Adelaide’s Health and Medical Sciences building on North Tce, in conjunction with the Royal Adelaide Hospital, researchers are exploring how it can be used to treat disease.
For those with hard to treat Type 1 diabetes, life can be extraordinarily stressful.
With extreme swings in blood sugar levels, and the ever-present threat of hypoglycaemia, some patients have to have another person with them at all times, in case they go into sudden shock.
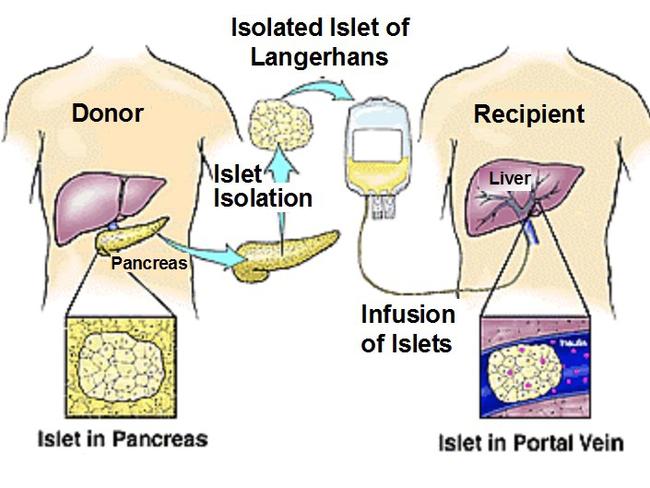
Currently, only severe cases of type 1 diabetes can be treated with an islet cell transplant from human donors into the liver.
While this restores the patient’s ability to produce insulin and regulate their blood sugar levels, it is hard to monitor the progress of the transplant once it is in the liver and also consigns the patient to a strict regime of anti-rejection drugs.
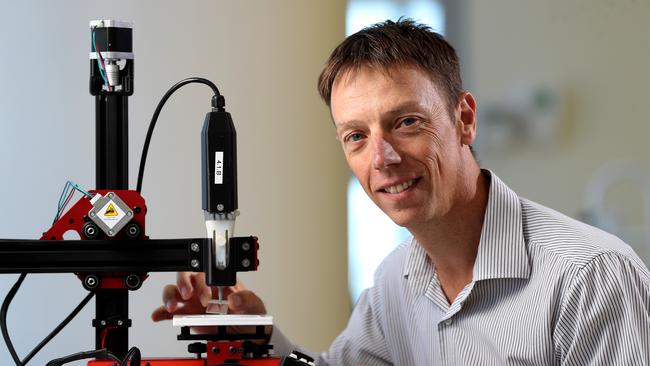
Principal medical scientist Chris Drogemuller, in a collaboration with the University of Wollongong, is using an islet 3D printer called the PICT pen (Pancreatic Islet Cell Transplant) to provide a complete new way for transplantation.
The PICT enables researchers to print three different cell types (islets, endothelial cells and regulatory T cells) and position them precisely within a 3D lattice structure which will be placed under the skin.
The sky is the limit for what other conditions might be treated through 3D printing.
The endothelial cells help the islet cells regrow their blood vessels (lost during the isolation process) which are crucial for their survival and function.
The blood vessels allow the islets to sense increasing blood glucose levels and then carry the secreted insulin to other cell types within the body signalling them to take up the glucose and remove it from the blood stream.
The regulatory T cells help modify the immune response to the transplanted islets preventing their rejection.
“The ability to 3D print these islet structures will mean that we no longer have to transplant the islets into the patient’s liver,’’ Drogemuller says.
“While the liver is the current site into which islets are transplanted it has several drawbacks. We can’t take a biopsy of the cells to see how they are going or to monitor rejection.
“The liver is exposed to the highest concentration of anti-rejection drugs which are toxic to the islet cells.
“Up to 50-70 per cent of islet cells die within the first 24 to 48 hours following transplant into the liver.
“This could be avoided potentially if transplanted under the skin.”
The structures take anywhere from several minutes to an hour or more to print, depending on the complexity and number of cell types, with an ‘ink’ made of several different components, the main one being alginate (a gel extract from seaweed).
It can also include other molecules that promote survival of the cells within the ink or improve their function, and anti-rejection drugs that are required to prevent the patient’s body from rejecting the islets that have been purified from a deceased organ donor pancreas.
While he can’t give an exact time frame on when the technology may be ready for human trials, Drogemuller is excited by the new technology and progress so far.
And he’s working on harnessing biological techniques used by another disease to potentially eradicate the need for anti-rejection drugs.
“3D printing provides several different approaches to minimise or completely remove the need for immunosuppressants,” he says.
“This can be achieved by incorporation of the drugs into the 3D structure to provide local immunosuppression and/or incorporating specialised immune cells capable of modulating or preventing recognition of the islet cells as foreign,’’ he says.
“Cancer tumours are very clever at avoiding detection by our immune system and hijack some of the immune cells to provide a cloak to protect it from immune attack and destruction.
“One of our strategies is to try to mimic this process using 3D printing to co-locate islets with these specialised immune cells to prevent immune detection and destruction.
“While 3D printing islet cells to treat type 1 diabetes has the potential to one day remove the need for insulin injections I see it as one of many new treatments that will be used to combat this disease in the future.”
The main advantage over insulin injections is the cells provide a physiological response to rising glucose levels, avoiding the large swings that can occur in type 1 diabetics managing their disease with injections, Drogemuller says.
“This will prevent the likelihood of diabetic comas and also reduce the risk of long term complications such as kidney disease, cardiovascular disease and nerve damage,” he says.
“The sky is the limit for what other conditions might be treated through 3D printing as evidenced by the scale and scope of research in all fields of medicine, for example, organ replacement, personalised bone replacement and medical devices.
“These are only a few examples of how far this technology has already come.”


Prawn gel probe spawns hope for back pain breakthrough
EVER battled peeling a prawn and wondered what it is about the shell that makes it so annoying to remove? Adelaide researchers believe a part of the shell that makes it strong but bendy could help ease excruciating pain after back surgery.
Using Netflix, Uber tech to keep flu outbreaks in check
COULD ‘big data’ technology used by Netflix and Uber be the key to getting a grip over influenza outbreaks? A team of Adelaide-based researchers is finding out.