SA doctors blame a culture of bullying and stress for crippling their mental health and endangering patients
Stressed doctors says South Australia’s broken hospital system is leaving patients at risk of poor care that could cost lives. Listen to this story as a podcast.

SA Weekend
Don't miss out on the headlines from SA Weekend. Followed categories will be added to My News.
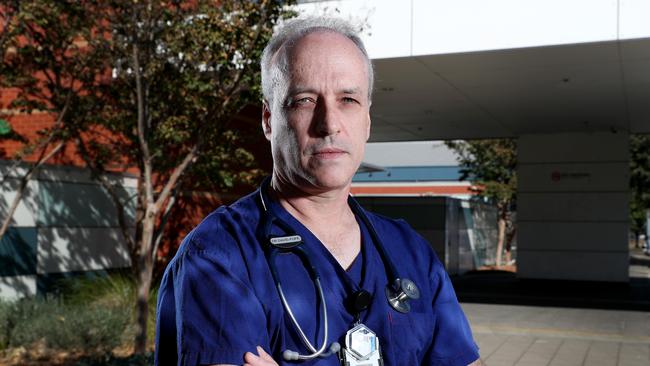
David Pope has worked some ridiculous shifts in his time as an emergency doctor. There was a period, when he first went to Lyell McEwin Hospital 21 years ago, when he’d start on Friday at 6pm and finish Monday at 9am.
Yes, there were supposed to be sleep periods but the emergency department of a big hospital is a cup of human frailty constantly being refilled – stopped hearts, overdosed veins, broken bones, blackened eyes, angry people, shattered lives – and rest is not always possible.
But the longer Pope went, the more his ability to make life-and-death decisions was degraded. “I was ordering medicines that wouldn’t make sense to anybody,” he says. “You’re almost in a stupor. Luckily the nursing staff had some insight.”
LISTEN TO THIS STORY IN PODCAST FORM
Despite the torrent of pain and suffering, he loved the work. It was, he says, an area where he felt he could do the greatest good, keeping people alive in the vital, early moments of their trauma. And he also knew he couldn’t possibly be bored.
“You never know what’s coming in the door and to this day you will encounter new things you’ve never seen before,” the emergency specialist says.
But what Pope did not enjoy was the pay. It seemed extraordinarily low for the hours he worked, so he investigated. “And I discovered that quite deliberately they weren’t paying us correctly,” he says.
“And then, because I’d discovered the errors, they without question paid me. But they didn’t do that for my colleagues who didn’t raise it themselves. And I thought that was egregious.”
So he surprised himself. Despite growing up on a farm where unions were despised, he joined the South Australian Salaried Medical Officers Association, or SASMOA. Today he is president.
But, he claims, wage theft is still a problem in the public hospital system – and one of a range of issues driving up stress levels among young doctors in particular, who say they are bullied, overworked and afraid of claiming overtime. Often, the bullying is by the senior doctors, but also it can be their workmates.
Pope’s union is now looking at a multimillion-dollar class-action claim against the State Government for back pay for the junior doctors. The legal enforcement of safe working hours – whatever they may be – could also be pursued. “I deal day-in, day-out, with some of the most traumatic things that human beings can ever experience and that doesn’t stress me at all,” says Pope. “But what does stress me is not being able to do my job properly: not being able to relieve suffering because of a system which stops you doing that, doesn’t make any sense, and is extremely inefficient.”
In interviews, young doctors in the public health system say stress levels go much deeper than pay. While none were prepared to be identified – we have used pseudonyms – for fear of losing their jobs, they told SAWeekend of constant fatigue, bullying, abuse, shouting matches between doctors and even falling asleep at the wheel of their cars from exhaustion. But what stressed them most of all, they said, was a lack of resources: too few staff, too few beds.

Just how few was demonstrated on March 20, when the Australian Nursing and Midwifery Federation counted what it said was a record 118 people waiting for a bed in Adelaide’s emergency departments – 11 of them for more than 24 hours.
The Health and Wellbeing Minister Stephen Wade’s office did not respond to an interview request, but the State Government says it’s tackling the problem, committing an extra $2bn in health spending since the last election, taking the annual budget to $7.2bn.
The Flinders Medical Centre ED was given an extra nine emergency doctors last year, and will become the biggest in the state with an $8.2m expansion. There’s also a $58m ED expansion at the Lyell McEwin, and an upgrade for the Queen Elizabeth Hospital’s ED as part of a billion dollar capital works expansion for the system. Yet stress remains widespread among hospital medical staff.
The latest AMA health check survey of young doctors in SA hospitals reveals many felt bullied or harassed at the big hospitals in 2020. Lyell McEwin was the worst with 64 per cent of those who took the survey reporting bullying or harassment, followed by the RAH at 55 per cent. Flinders was rated best with 33 per cent.
Yet 80 per cent of Flinders doctors said they feared complaining would only lead to negative job consequences, slightly above the rate at the other big hospitals.
Fatigue was another big concern. At the RAH, 92 per cent of young doctors said they were concerned about their personal safety due to fatigue, and 85 per cent said they worried about making a medical error from feeling too tired.
“The RAH has this false reputation for being a centre of excellence,” one young doctor said. “It rides on staff working for free and beyond the scope of their practice in order to function.”
Other surveys, including one by Beyond Blue, have found doctors are more prone than average to mental health issues such as anxiety and depression – and those under 30 are the most vulnerable, with young women the most at risk.

Jemma, a young doctor in her 30s in a busy Adelaide emergency department, knows all about fatigue. She says she struggles not just with the workload and impact on patients but a system that thinks it can operate on inadequate resources.
“What surprises me is that we don’t have more beds,” she says. “Given the ageing of the population and the complexity of the patients, we need more.
“We’re seeing situations where we’re trying to get people into hospital and we’re looking at three, four weeks to bring them in … just because there’s no beds.”
The media has focused recently on ambulances, she says. “But I think it may be missing the point: the reason why there are no ambulances, and why there is ramping, is there’s no space in hospital.”
Jemma loves what she does, and feels privileged to do it, but she sometimes questions why she keeps at it.
“I think stress levels are really high,” she says. “I’ve asked myself, why am I doing this job? Why am I in a situation where I’m having to try to talk to people in the middle of a waiting room? And why am I in a situation where I can’t even promise someone a bed in the hospital, and they’re dying?
“For me, it keeps coming back to the fact that I’m here for the patients. I’m here trying to do the best I can. But it’s damaging and people are just exhausted.
“I’ve seen colleagues collapsing at work. I’ve seen colleagues have to be admitted to hospital on their days off because they’re just exhausted.”
She also sees, regularly, colleagues shouting at each other as they try to do their jobs. It can be frightening, she says, to call another doctor in the middle of the night for advice. They may be working one night in three on call, possibly needing to come into the hospital, and then do their normal shift the next day.
“And if you need help because you’re on night shift, you know, they can become very angry if they think that you’re calling for a stupid reason,” she says.
“They can yell at you. It can be shocking; they’ll just snap at you and tell you off – ‘Why are you asking me this question? You should know better’.”
Lily is another emergency doctor who has seen the impact of the stress. “I’ve only had one of my medical colleagues suicide,” she says.
“That was a senior doctor, but I certainly think the stress of the job was a contributing factor. And many friends I went to medical school with, they’ve struggled.”
But she says it’s not the patients and their heartbreaking stories who make her stressed – they are what keep her going.
“No, it is the system in which I have to work,” Lily says. “That is the issue. And we feel powerless to do anything. I think that’s one of the biggest things and most important things to think about. Things are done to me and to my work without my say and I just have to get on and do it.
“Every medical college and hospital system says we want our training medical officers to sit on our committees and be part of it, but we’re not given the time to do it – so how can we be part of improving the system when we are working in it, but we’re excluded from it?”
But junior doctors are vulnerable, she explains, because they are trying to advance their careers. They may want to become surgeons, and so need to be selected for training – so they need to liked, impress the doctors who make decisions, and accept what may be bullying behaviours.
Complaining about working overtime, or complaining they were not paid for it, could sabotage their career prospects.

“There’s a lot of reasons for people not to speak out,” she says.
For female doctors it can be even more difficult because flexible working arrangements for women with children may not be available. “One woman (doctor) checked to see if there would be someone to cover for her if she had a baby and was told no,” she says. “Another pointed out in the intensive care section of her hospital, there were no senior women consultants or intensive care specialists.”
The problem, she suspects, is that it was run by men who had never needed the flexible arrangements to accommodate their families and children.
The biggest issue for hospitals, though, was the ageing of the population which meant more people were coming through with increasingly complex medical problems. “And the health service has not kept up with demand,” she says.
“We’ve got the wards full of patients that are sicker and need longer treatments. And we probably need more doctors and nurses and more beds. And we need more community care facilities so that we can admit patients to hospital.”
Most of younger patients are seen and sent home, she says. “It’s people over the age of 70 and 80 who tend to be admitted to hospital because they accumulate diseases through their life.”
But it is not just the elderly who clog the system. The Women’s and Children’s Hospital has been coping with a COVID baby boom that has tested its capacity. But, alleges one doctor, the understaffing levels there are diabolical and potentially life-threatening.
“It’s getting to the point where providing quality care is almost impossible,” this doctor says.
“I just really feel like it’s getting to the point, particularly overnight, where it’s not safe, because of the number of deliveries that we’re doing.”
Staffing ratios are highest during the day, but overnight may drop to three doctors for up to 90 patients.
“And you have to ask, if you’re providing a 24-hour service, and you’ve got high acuity patients, how is that? Like, how has the hospital allowed that to happen? And I honestly think it won’t be until there’s a maternal death that’s preventable, or something really drastic that happens, that the executive will find more funding.”
But maternal death is a very uncommon event in a rich country? “Yes,” the doctor says. “But do I think that could happen at the Women’s and Children’s? Yes, I do. Because you haven’t got enough staff, the staff that you have got have been flogged, and they’re tired. And when you’re tired, you know, your ability to make good decisions is to a degree inhibited.”

The real danger would be concurrent emergencies, with not enough staff to look after both sets of patients. “The end of last year was getting really tough because people were calling in sick, which is absolutely their right, but then for the people left working at the hospital there’s no process for getting locums or additional doctors to help fill shifts,” the doctor says.
That meant those left had multiple tasks like the women’s assessments, covering the ward, and emergency theatre cases.
“And that’s a job that might normally be done by three people, but then it falls to one person. And you can imagine that you end up providing a pretty crappy level of care to women … who miscarry, or are having complications with their pregnancy, or have had a traumatic birth.
“And it’s really hard to spend the necessary time consoling them and, you know, providing gentle appropriate care when you’re thinking, ‘Oh, shit, I’ve got to do seven other jobs’.”
Is it just about money? No, this doctor says, it’s “a huge disconnect between the reality of what’s needed and the executive making the decisions”.
Stress within the health system was examined by a state parliamentary inquiry in 2019, which made more than two dozen recommendations to cut workplace fatigue and bullying in hospitals.
It found the high-pressure nature of the work, coupled with long hours, shift work, overtime and on-call work “creates an environment that places health professionals at greater risk of workplace fatigue and bullying”.
That was made worse, the report said, by a poor workplace culture stemming from a hierarchical workforce and lack of management skills among many clinical leaders. For some doctors it was too much.
One told the committee: “There is an entrenched culture of mistreating trainee medical officers throughout SA Health which perpetuates the bullying and burnout of our young doctors.
“The only time I ever complained about excessively onerous rostering I was told in writing, ‘It doesn’t matter what’s in your enterprise bargaining agreement, this is what is expected of you’ by the Director of Physician Training at a (city) … hospital. I was so exhausted and demoralised by that stage that I didn’t have the will or the strength to escalate the complaint, I just quit my job.”
One of the key recommendations made by the committee was that the bodies that run the hospitals – the Local Health Network boards – be made accountable for the management of staff fatigue and bullying. But while it may be possible to measure things like complaints (although they are rarely made), staff satisfaction, absenteeism, turnover and overtime levels, how do you fix the problem?

Professor Michelle Tuckey of the University of South Australia’s Centre for Workplace Excellence has designed a tool to audit the risk factors for workplace bullying, and after identifying where the problems are, to fix them. It’s been embraced by the parliamentary committee, the Australian Medical Association and SASMOA – but while the tool was tested and validated at Flinders Medical Centre, and has been used in a few select locations, SA Health has not engaged Tuckey to work on the broader system.
“Bullying is all about repeated exposure to unreasonable behaviour,” she says. “And it’s surprising to some people to learn that it really shows up as work-related behaviours rather than personal attacks like rumour-spreading or name-calling,” she says.
“Bullying is an organisational issue not a personal one … it’s actually the work environment that provides the fertile soil for bullying to thrive, and has the ingredients motivating bullying in the first place.”
Bullying and stress grow together from the same causes which in the case of the hospitals can be fatigue, tight budgets, work overload and lack of time for positive things like professional development.
With doctors, bullying is often experienced as unjustified criticism, lack of recognition, or having their work devalued or undermined. “The good news is that these things – recognition, performance feedback, appreciation, support – are modifiable,” Tuckey says.
Her system can identify wards that are riskier, with higher levels of staff reporting bullying, absenteeism, higher patient-related errors and higher work injuries. “We independently worked out which wards were having really good outcomes and which wards were having risky outcomes for both patients and staff,” she says, “and these outcomes corresponded with predictions from the risk audit tool”. That allows changes to be made and monitored by improving work systems and practices that help make wards bullying-resistant.

AMA president Dr Chris Moy, who organised a bullying and fatigue summit last year, sees them as cancers in the health system. He’s called out the RAH culture as toxic and said in the case of SA Health, “the fish rots from the head”. He is a big supporter of Tuckey’s ideas, which, he says, adopt a scientific approach that takes the guesswork out of the problem.
As well, he has won support from the State Government to amend health legislation so the hospital boards must promote a healthy workforce culture and reduce harassment and bullying. “That puts them much more in line with normal corporate boards,” Moy says. “Because currently, if you’re a corporate board, if somebody is bullied or somebody commits suicide due to psychological problems caused by your workplace, you’re responsible. But there hasn’t been that in our hospital boards.
“Until now, it’s more been about just providing care for patients and maintaining budgets, but not caring for your staff. This is a fundamental change.”
Junior doctors in hospitals make up a big slice of those who seek help from Doctors Health SA, set up to help troubled members of the medical profession. But older specialists and GPs also seek help says Dr Roger Sexton, who runs the not-for-profit.
Sexton only treats doctors, either at a city clinic or through a 24-hour help line – 8366 0250. The clinic treated 500 doctors last year, up 25 per cent, while those calling the emergency line doubled to 100 due to COVID stresses such as worrying about bringing the virus home to the family.
“Most of the calls were urgent,” Sexton says. “They were doctors in immediate distress. Some were required to stop work for a time.”
He says the number of doctors who report thinking of suicide or – more rarely and seriously – planning it, is concerning. The service has helped many doctors who were planning to kill themselves, he says. “We’ve definitely helped dozens.”
David Pope says the shifts today tend not to be as crazy as he used to work, but the hospitals are busier so “fatigue is as bad as it’s always been”.
“Many units are understaffed so people are doing extra shifts just to keep services running – and where they used to run hospitals at around 85 per cent capacity, they now try to run them at over 100 per cent. Essentially the workload exceeds the labour available.”
While Pope does not say how many more doctors are needed, he says demand will continue to grow as the number of 80-year-old Australians grows from 500,000 today to 1.5m by 2058. Modelling he has seen predicts demand growth of 5 to 8 per cent every year for the next decade at least. “The bottom line,” Pope says, “is the system needs more resources.”
For help with emotional difficulties contact Lifeline on 13 11 14, lifeline.org.au, or for help with depression contact Beyond Blue on 1300 224 636, beyondblue.org.au



