World-first needle-free treatment that could save allergy patients
People with deadly allergies could receive life saving, needle-free treatment from a breakthrough Australian medical device being developed, with plans for more trials to begin within months.

Wellbeing
Don't miss out on the headlines from Wellbeing. Followed categories will be added to My News.
People with deadly allergies could receive life saving treatment without a needle from a groundbreaking medical device developed in Brisbane that could work up to eight-times faster than injection alternatives.
It’s hoped Australian clinical trials using the device could begin on allergy sufferers within months.
But the team behind the revolutionary inhaler designed to treat anaphylaxis need a further $10 million in funding, or Australia risks losing the world-first device to overseas investors.
A shot of adrenaline used to treat anaphylaxis is currently delivered by painful needles like EpiPens or Anapens.
De Motu Cordis Pty Ltd (DMC) has been developing its simple, single-use inhaler, about the size of a pencil sharpener, that is designeddeliver adrenaline in a fine dry powder form.
Pulling the red cap off automatically activates the device containing the lifesaving drug, which can reach deep into the lungs by inhaling.
Phase one clinical studies have shown the unique powder formula reached peak absorption in healthy volunteers up to eight times faster than a liquid adrenaline autoinjector.

Emerging stability data also suggests the inhaler may have a shelf life longer than some autoinjectors when stored at room temperature.
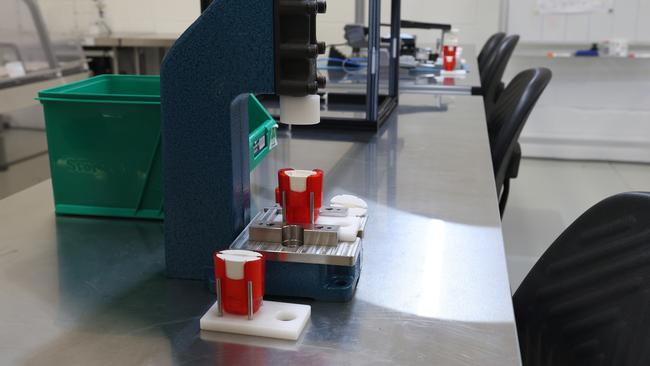
DMC’s deviceis being created and tested in a small lab in Windsor, in Brisbane’s inner north.
There, a small team has been simulating human breaths to test the lung inhaling capacities of potential patients, 3D printing various designs to improve usability and to check how quickly the device’s cap can be removed in an emergency.
There have been six prototypes so far with what is hoped will be the final design now ready for further clinical trials.
An onsite workshop has also been testing the production, assembly and packaging of the device.
For device project lead Ben Trout, his work at DMC over the past five years has been personal.
His daughter is anaphylactic and she first required an autoinjector at just eight-months-old.
“As a parent, you never want to cause your child pain, you know what you’ve got to do, but it doesn’t stop the thought ‘I’ve got to inject a needle into my child’s thigh’,” he said.
“Seeing a child in distress is something no parent should have to see.”
The device will need to be approved for adult use first.

Professor John Fraser AO, who is St Andrew’s War Memorial Hospital’s Director of Intensive Care Unit, is DMC’s founder and Chief Medical Officer.
The company also has two high profile backers in former Wallabies captain John Eales AM as chair and Greencross Vets founder and Shark Tank investor Dr Glen Richards as non-executive director.
Prof Fraser said he was inspired to create a device that could administer adrenaline faster after seeing heart attack survivors left with brain injuries from a lack of oxygen during cardiac arrest.
He then pivoted thatsame concept to target anaphylaxis patients.
“I thought if we can use the fact that the lungs are the perfect drug delivery system, if I could get the drugparticles small enough to get it down there, then an inhaler is the way,” he said.
Chief Scientific Officer Dr Sean Dalziel said the formulation of the drug into an encapsulated crystalline powder took months, with the process so innovative DMC has secured a US patent for it.
“We had to do some work on how to take just the bulk adrenaline, to modify that through specialised milling technologies to bring the particles down into a size, shape and crystallinity, which was ideal for what we wanted to be absorbed via the lung,” he said.
“Then we needed to mix that with other powders to make it stable, reproducible, and manufacturable.”
Dr Dalziel said prototype testing of the powder had shown it lasted up to three years without degrading or losing potency, and he thinks that could be extended even further.
“In our stability results, we’ve already more than doubled the period of time of which some autoinjectors would typically lose their shelf life and go off and we’re continuing,” he said
“We’re going to aim for a couple of years longer.”
Drug Project Leader John Fredatovich, who oversees DMC’s clinical programs, said about 50 healthy Australian patients without allergies had used the product so far over two clinical trials to test the safety and tolerability of the drug.
A third pilot trial, planned to begin in coming months, will now test the effectiveness of the device on patients with allergies.
“We will actually be using it in a clinic with patients that may experience anaphylactic reactions, and it’s there as an option to treat that,” he said.
“It will give us an understanding of how patients react and respond to the medication, their heart rate and blood pressure and so we can start to gather data.”
Prof Fraser said his team were seeking $10m in funding to complete the trial.
“I hope this trial will stimulate international interest and then bring in the big bucks, which will allow us to start doing the work to get the product to market and produce jobs in manufacturing for Queensland and Australia,” he said.
“If we can get this device into people’s hands I’m so very hopeful that an Aussie product will save lives – not just here but across the globe.”

Prof Fraser said Australia punched well above its weight in medical research but had “dropped the ball” when it came to device development.
It comes after Brisbane biomechanics engineer Dr Daniel Timms was forced to turn to the US for start-up funding for the world’s first permanent artificial heart replacement, which he created in his northside Brisbane home.
The heart implant from BiVACOR, a company Prof Fraser helped co-found more than a decade ago, was developed in the early 2000s by Dr Timms in a desperate bid to save his father who was suffering heart failure and has sadly since died.
After years of work in Queensland, Dr Timms found support for his invention in the US, who now lay some claim to the device.
This week it was revealed that, in November, doctors completed Australia’s first BiVACOR heart implant surgery on a man in his 40s at St Vincent’s Hospital in Sydney.
The patient then received a donor heart transplant in early March and is recovering well, marking the longest time a patient has lived between receiving an artificial heart and a donor transplant.
Prof Fraser said the BiVACOR example showed why Australia needed to better support and fund its own medical technology developments.
He said there needed to be a movement to “Make Australia Make Again”.
“What we realised during Covid was that we make almost no med tech products,” he said.
“As someone with five kids, I want good jobs in Queensland, and I also want to see this as something that Queensland has given to the world.
“Let’s use our ability, innovative spirit and translate that world leading research into dollars and jobs.”
Lylah Ricks is a sufferer of serious allergies who could benefit from the device. The almost five-year-old is allergic to eggs, peanuts and dairy and is still undergoing tests for more.
Her life has been saved three times by a painful EpiPen injection after suffering potentially deadly anaphylaxis.

DMC CEO Peter O’Neill said his team were proud of the company’s Australian and Queensland heritage.
He said the intention was to establish DMC’s global hub in Brisbane to continue development efforts to fully use the technology and its potential, which could include multiple products and applications over the coming decade and beyond.
“We’ve had great support here, and now, because we’re on the international radar, there is globalinterest, and it is important to entertain that if it’s going to sustain your business” he said.
“We’d prefer to avoid the situation, where everyone looks back in five- or 10-years’ time and says, ‘why didn’t we just support that ourselves locally because look at where they’ve got to now and how many patients they are helping’.”
He said the company would be aiming to secure U.S. Food and Drug Administration approval first before seeking subsequent approvals from other countries including Australia’s own Therapeutic Goods Administration.
“It is important to be targeting the largest commercial market opportunity in the world,” he said.
“This credibility assists all of our further global plans.”
Originally published as World-first needle-free treatment that could save allergy patients



