Where STIs are rising in Australia
Australia is grappling with a hidden epidemic of sexually transmitted infections, experts warn. See the interactive map to view the areas with the biggest increases.
Sexual Health
Don't miss out on the headlines from Sexual Health. Followed categories will be added to My News.
Australia has a hidden epidemic of sexually transmitted infections that needs an urgent and coordinated emergency response as cases spike across the country.
Sexual health experts warn that fewer people are wearing condoms and testing rates have failed to pick back up since Covid due to the difficulties of getting in to see an affordable doctor.
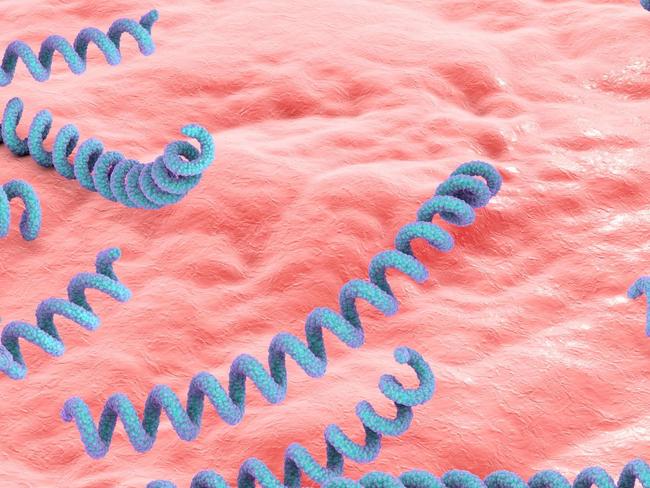
Rates of STIs are surging with syphilis infections up 600 per cent in 15 years in parts of Queensland alone.
Analysis of the most recent national STI data published this month from UNSW’s Kirby Institute shows that the notification rate of syphilis grew in 277 out of 311 measurable locations over seven years.
For chlamydia, the rate went up in 171 of 331 places that could be compared.
Meanwhile, gonorrhoea rates increased in more than 90 per cent of locations.
Adelaide’s city region had the biggest increase of chlamydia rates in the nation over the last seven years, followed by Stonnington West in Victoria which is made up of the affluent areas of South Yarra, Toorak, Armadale and Windsor.
Western Australia and the Northern Territory are battling an outbreak of syphilis that’s disproportionately affecting Aboriginal and Torres Strait Islander communities.
However, outside of this, the biggest increase for infectious syphilis was seen in the Gold Coast’s Southport region, which had 25 cases for every 100,000 people in 2016 but in 2023 had 127.
The map below shows the rate per 100,000 people and the absolute increase and percentage increase between 2014-2016 and 2021-2023:
The Yarra region in Victoria, which includes Richmond and Collingwood, had the biggest increase in gonorrhoea over this period for a city area.
In NSW, Sydney Inner City topped the list for having the highest proportion of syphilis cases – 216 per 100,000 people – in the state.
The next highest was the Marrickville, Sydenham and Petersham region followed by Botany in the city’s south.
The Eastern Suburbs North region, which includes Bondi, Double Bay and Paddington, had the second highest notification rate of chlamydia, only behind Sydney Inner City.
In Queensland, after Southport, the Central Highlands had the highest rate of syphilis, followed by the Gold Coast Hinterlands.
Brisbane North and Brisbane Inner had the fifth and sixth highest rates after Queensland North.
State figures show Queensland recorded 1467 cases of syphilis last year, which was an increase on the previous year.
In Tasmania, total gonorrhoea cases quadrupled between 2016 and 2023, with the Central Highlands seeing the biggest increase, followed by Hobart inner, Hobart’s north east then Hobart’s north west.
The Meander Valley-West Tamar region recorded the highest increase in chlamydia rates in Tasmania, however most areas of Tassie saw a significant reduction in cases over the past seven years.
Tasmania’s Central Highlands recorded the biggest increase for syphilis in the state, which had eight cases for every 100,000 people in 2016 but in 2023 had 20.
The map below shows the rate per 100,000 people and the absolute increase and percentage increase between 2014-2016 and 2021-2023:
Monash University Professor Jason Ong – the director of Australia’s largest public sexual health clinic run by Alfred Health in Melbourne – is the lead author of a new international STI study published in the May issue of eClinical Medicine.
It highlights that with 374 million new curable STI bacterial cases annually, World Health Organisation targets to curb the global epidemic are “a long way” from being met.
Across Australia there has also been an alarming increase in babies dying from congenital syphilis after being infected in the womb by their mothers.
Untreated, around half of these congenital syphilis infections end in miscarriage, stillbirth, neonatal death or permanent disability.
Dr Belinda Hengel, a Kirby Institute researcher at the UNSW, said they had found a heartbreaking 25 per cent of the babies born with congenital syphilis were stillborn.
The map below shows the rate per 100,000 people and the absolute increase and percentage increase between 2014-2016 and 2021-2023:
She said there had been a significant amount of work done to decrease the gaps in access to antenatal care and increase testing women for syphilis within antenatal care.
“In 2024 there were six cases reported, down from 20 the year before. However, even one case of congenital syphilis is too many,” the researcher said, adding it was preventable and even one case represented a failure in our health care system.
“We need to understand what strategies have worked to improve rates of syphilis screening, particularly for women of reproductive age, and scale up these strategies nationally where relevant.
“Within urban and regional areas, access to care for individuals who experience disadvantage is leading the rise of cases. Publicly funded sexual health services and outreach services are the key to improving testing coverage.”
Why are STIs rising?
Experts are concerned that despite the serious consequences for sexual, reproductive, and mental health, control efforts for STIs often focus on individual-level interventions like condom promotion and behaviour change, which this latest study says is insufficient.
The international researchers say effective strategies should focus on expanding access to quality sexual health care, rapid testing with same-visit treatment and diagnostics that utilise AI technology.
Professor Ong said hardly anyone was using condoms and this had led to increased rates of STIs.
“It is for a variety of reasons, predominantly driven by things like people are no longer in fear of getting HIV,” he said.
“They also think an STI is curable so they don’t mind getting it. So they drop the condoms. Condom campaigns have also been underfunded in recent years.”
He said to control STIs more effectively, there needed to be a shift to prioritising accessible, stigma-free health services, leveraging technological advances and investing in comprehensive public health policies.
Kirby Institute epidemiologist Skye McGregor said people dropped off getting tested during Covid and they hadn’t seen it rebound.
“With young people we know STI screening is below where we’d like to see,” Dr McGregor said.
“Asymptomatic screening is not very high, so people are unaware they are transmitting it.”
She said the difficulty getting in to see an affordable doctor was a barrier to getting tested.
“Access to healthcare providers was substantially impacted by Covid but we’ve seen that continue,” she said.
“So it’s hard to get an appointment quickly with the GP, it’s very hard to get an appointment at sexual health clinics that have free or very-low cost testing.”
Professor Ong said there had been an under-investment in our health systems.
“For example, in Victoria, the Melbourne Sexual Health Centre is the only sexual health clinic for the whole of Victoria, so we are meant to be serving around five million people which is almost impossible,” he said.
“Whereas NSW has about 30 sexual health clinics, so there’s a big disparity across states.”
But Professor Ong said additional sexual health clinics were not the full answer to the problem.
“I think there’s stigma around this topic. So even though you have so many clinics, if people don’t feel comfortable attending the clinics, they won’t turn up,” he said.
“We need to think about the structural changes that need to happen rather than focus on a blame game.”
Treatment
Royal Australian College of General Practitioners Sexual Health Medicine Chair Sara Whitburn said STI testing was a core part of GP practice.
“GPs are well equipped to offer this service. Sexual health clinics are also there for GPs to refer to if needed,” Dr Whitburn said.
“To do sexual health well, GPs do need to have adequate remuneration for longer consults, those 20-minute plus consults. That’s another reason that reviewing and increasing Medicare rebates for longer, holistic care is so important.”

To this end, the RACGP is calling for a commitment from all political parties for a 40 per cent increase for GP consultations lasting between 20 and 60 minutes.
The professional body for general practitioners in Australia says these are increasingly what’s needed among patients, and what is driving a lot of GPs scepticism of the parties’ bulk billing incentive commitments.
Dr Whitburn said a new rapid test kit test allowed women to self-screen for chlamydia and gonorrhoea.
Originally published as Where STIs are rising in Australia


